Get the free North Carolina Pharmacy Prior Approval Request form
Get, Create, Make and Sign north carolina pharmacy prior
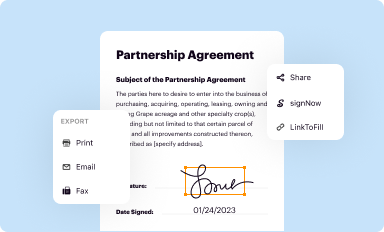
Editing north carolina pharmacy prior online
Uncompromising security for your PDF editing and eSignature needs
How to fill out north carolina pharmacy prior
How to fill out north carolina pharmacy prior
Who needs north carolina pharmacy prior?
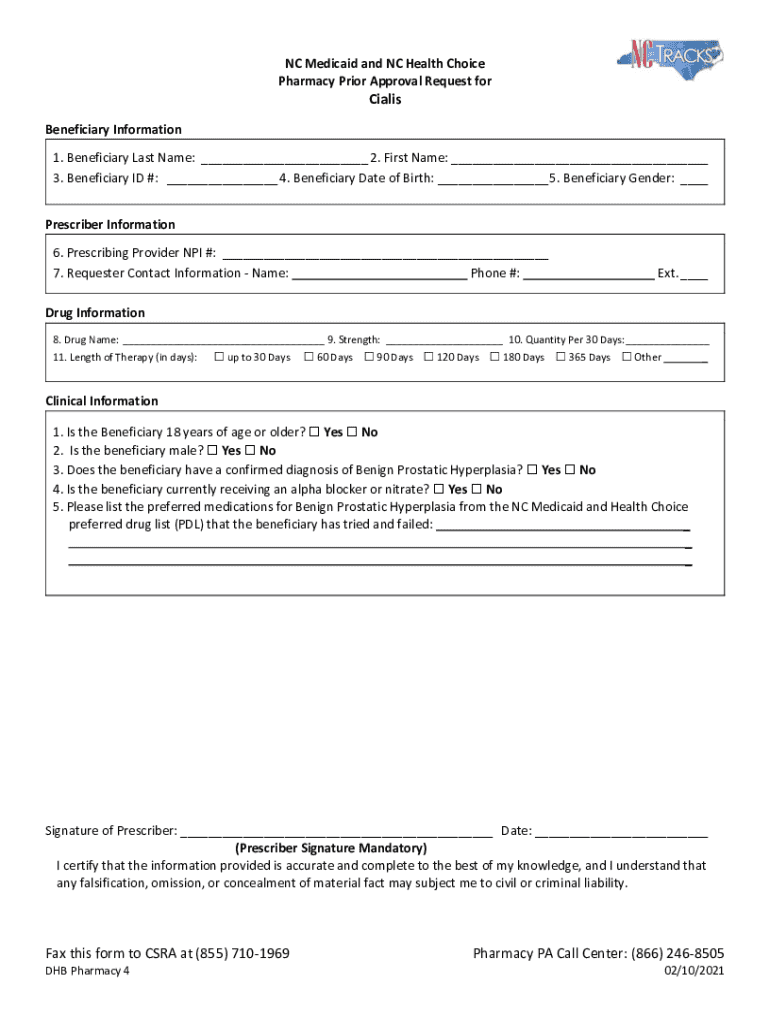
Understanding the North Carolina Pharmacy Prior Authorization Form
Overview of the North Carolina Pharmacy Prior Authorization Form
The North Carolina Pharmacy Prior Authorization Form serves as a critical tool in managing medication access. Its primary purpose is to obtain approval from insurance providers before certain medications can be prescribed or dispensed. This practice not only protects the interests of insurance companies but also ensures that patients receive treatments that are medically necessary and cost-effective.
Prior authorization is particularly vital in healthcare as it balances the need for innovative treatments with cost containment. Patients benefit from this process, as it can lead to coverage for medications that may not otherwise be included in their health plans. Common scenarios requiring prior authorization include expensive specialty drugs, off-label medication use, and specific health conditions like cancer or rare diseases.
Understanding the prior authorization process
The prior authorization process can seem daunting, but breaking it down into steps makes it manageable. First, healthcare providers or pharmacists identify which medications require authorization based on insurance requirements. Once identified, the actual request can begin.
Once the submission is completed, waiting for approval can take time. Typically, patients should expect a response within a few days, although this can vary by insurance provider. Pharmacists, prescribers, and insurance representatives play essential roles throughout this process, all working collaboratively to ensure patients have access to the medications they need.
Navigating the North Carolina Pharmacy Prior Authorization Form
The North Carolina Pharmacy Prior Authorization Form can be intimidating at first glance. However, knowing its structure and requirements eases the process. The form includes several sections that need to be accurately filled out to avoid delays in approval.
Completing each section accurately is crucial. Misentries can lead to denials or delays—common mistakes include omitting information and failing to provide sufficient clinical rationale. Taking the time to verify all information before submission can mitigate these issues.
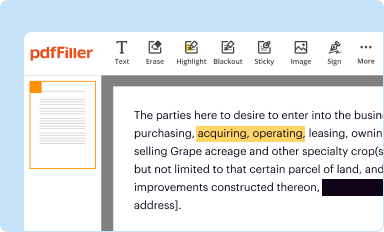
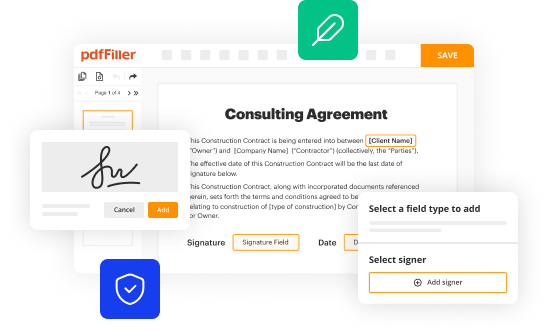
Interactive tools for completing the prior authorization form
Utilizing interactive tools like pdfFiller can greatly enhance the experience of filling out the prior authorization form. pdfFiller provides users with an easy-to-navigate platform that streamlines the entire process.
By leveraging these features, healthcare professionals can improve their efficiency in managing prior authorization requests.
Managing prior authorizations and document tracking
After submitting the prior authorization form, it’s important to keep track of its status. Patients and healthcare providers should maintain open lines of communication with insurance companies.
Proper documentation can be invaluable should any issues arise during the approval process.
FAQs about the North Carolina Pharmacy Prior Authorization Form
Understanding common questions regarding the North Carolina Pharmacy Prior Authorization Form can ease anxiety surrounding the process.
Being informed about these aspects helps to navigate the process effectively, ensuring the patient receives their needed medications without unnecessary delays.
Resources for patients and healthcare providers
Access to relevant resources is key for both patients and healthcare providers navigating the North Carolina Pharmacy Prior Authorization Form.
These resources can be invaluable in ensuring that the process of obtaining necessary medications is as smooth and quick as possible.
Case studies and real-life examples
Learning from the experiences of others can provide insights into effective use of the North Carolina Pharmacy Prior Authorization Form. Success stories highlight instances where comprehensive clinical information and timely follow-up led to the quick approval of necessary medications.
These case studies underscore the importance of thorough preparation and proactive management of prior authorizations.
Conclusion of the prior authorization process: Post submission
Successfully navigating the prior authorization process requires attention to detail from submission to approval. Key takeaways include being thorough in information gathering, maintaining clear communication with insurance providers, and understanding the implications of prior authorization on patient care.
Being informed empowers both patients and healthcare providers, ensuring a smoother experience in managing ongoing treatment needs.






For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
How can I edit north carolina pharmacy prior from Google Drive?
How do I make edits in north carolina pharmacy prior without leaving Chrome?
How do I edit north carolina pharmacy prior on an iOS device?
What is north carolina pharmacy prior?
Who is required to file north carolina pharmacy prior?
How to fill out north carolina pharmacy prior?
What is the purpose of north carolina pharmacy prior?
What information must be reported on north carolina pharmacy prior?
pdfFiller is an end-to-end solution for managing, creating, and editing documents and forms in the cloud. Save time and hassle by preparing your tax forms online.