Get the free cobra election notice - CalHR - CA.gov
Get, Create, Make and Sign cobra election notice
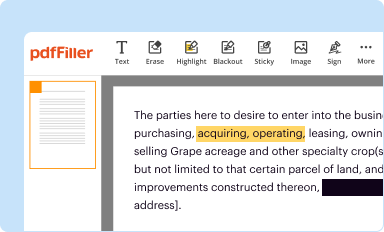
Editing cobra election notice online
Uncompromising security for your PDF editing and eSignature needs
How to fill out cobra election notice
How to fill out cobra election notice
Who needs cobra election notice?
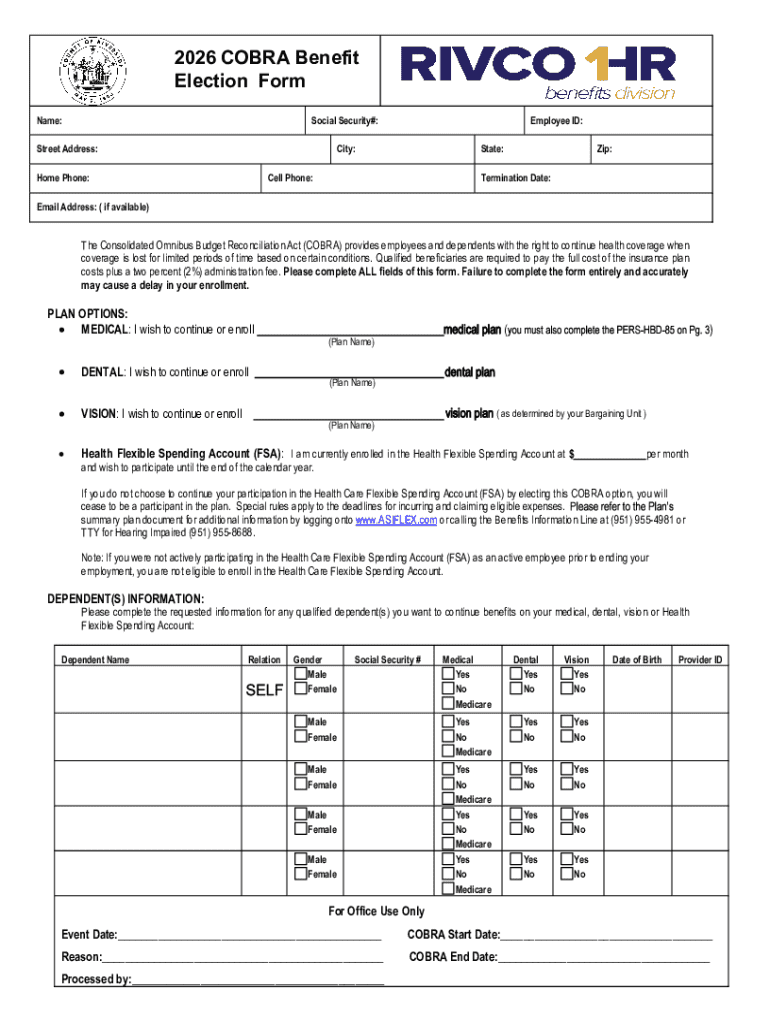
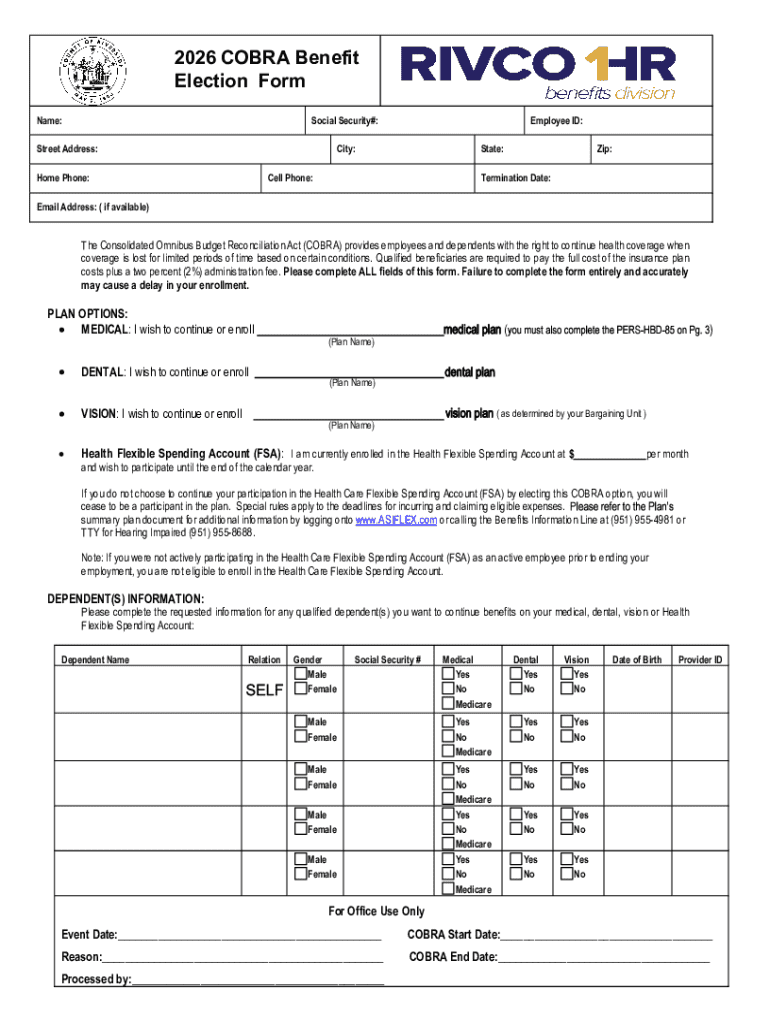
Understanding the COBRA Election Notice Form
Understanding COBRA health insurance
COBRA, or the Consolidated Omnibus Budget Reconciliation Act, offers individuals and families the option to continue their employer-sponsored health coverage after certain qualifying events, such as job loss or reduction in work hours. This program, enacted in 1985, provides a vital safety net for many Americans, ensuring they have access to necessary healthcare services without immediate interruption.
Eligibility for COBRA insurance
Not everyone is eligible for COBRA coverage. Eligibility generally includes employees who worked for a covered employer, with a qualifying event leading to loss of coverage. These events may include termination of employment, reduction in work hours, or other significant life changes. Understanding your eligibility is crucial to accessing COBRA benefits and ensuring necessary medical care.
The Cobra election notice form explained
The COBRA Election Notice Form is a crucial document that allows individuals to opt for continued health insurance coverage under COBRA guidelines. When a qualifying event occurs, this form is filled out to formally elect COBRA coverage, thus securing an essential healthcare lifeline during a vulnerable period.
This form is pivotal not only for employees but also for employers, as it ensures compliance with COBRA requirements and safeguards the rights of individuals seeking coverage. It is essential to fill out the COBRA Election Notice Form completely and accurately to avoid any issues when claiming your benefits.
Navigating the Cobra election notice form
Filling out the COBRA Election Notice Form doesn’t have to be daunting. A clear step-by-step approach can simplify the process. Below is a guide to help you navigate the form effectively and efficiently, ensuring that all necessary details are correctly captured.
Tips for filling out the Cobra election notice form
Completing the COBRA Election Notice Form can sometimes result in misunderstandings or errors, so it's wise to be meticulous while filling it out. Having clear and concise documentation avoids potential delays or denials in your coverage.
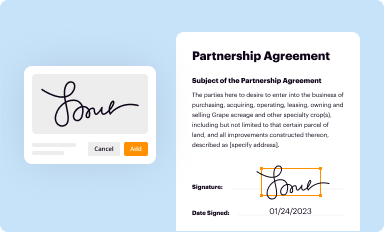
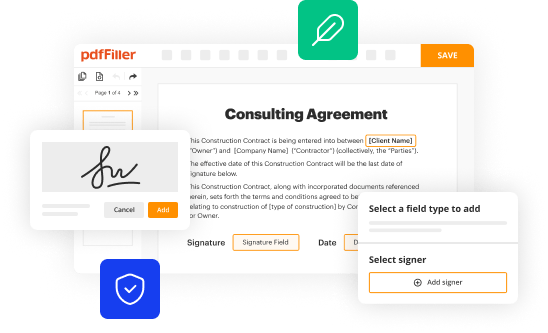
pdfFiller features a user-friendly interface that allows for seamless form management, enabling users to complete the COBRA Election Notice Form easily. Its interactive tools help make the process smooth, reducing stress and ensuring compliance.
Submitting the Cobra election notice form
Once you’ve diligently filled out the COBRA Election Notice Form, the next step involves submission. It's critical to understand the correct method of delivery to ensure your form is received and processed promptly.
Post-submission steps
After submitting your COBRA Election Notice Form, it's important to comprehend your rights and next steps. Monitoring your health insurance provider's communications can provide insights into your coverage status.
Frequently asked questions about the Cobra election notice form
When dealing with health insurance matters, having your questions answered is vital. Here, we address several common queries related to the COBRA Election Notice Form that can help clarify the process.
Interactive tools for managing COBRA coverage
Using pdfFiller as your document management platform simplifies not only the filling out of the COBRA Election Notice Form but also ongoing management of your health insurance documents. The platform provides numerous features to facilitate a smoother experience.
Ensuring compliance with COBRA regulations
Compliance with COBRA regulations is essential for both employees and employers. For employees, understanding your rights under COBRA can make a significant difference in securing necessary healthcare. Employers must adhere to specific guidelines to ensure employees are informed. Non-compliance can lead to penalties and loss of coverage for affected individuals.






For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
How do I execute cobra election notice online?
Can I sign the cobra election notice electronically in Chrome?
How can I edit cobra election notice on a smartphone?
What is cobra election notice?
Who is required to file cobra election notice?
How to fill out cobra election notice?
What is the purpose of cobra election notice?
What information must be reported on cobra election notice?
pdfFiller is an end-to-end solution for managing, creating, and editing documents and forms in the cloud. Save time and hassle by preparing your tax forms online.