Get the free 6. CLAIMS EDI PROCESSING PROCEDURES A. Claims EDI ...
Get, Create, Make and Sign 6 claims edi processing
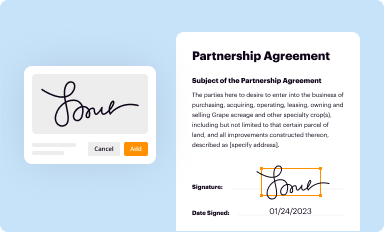
How to edit 6 claims edi processing online
Uncompromising security for your PDF editing and eSignature needs
How to fill out 6 claims edi processing
How to fill out 6 claims edi processing
Who needs 6 claims edi processing?
A Comprehensive Guide to the 6 Claims EDI Processing Form
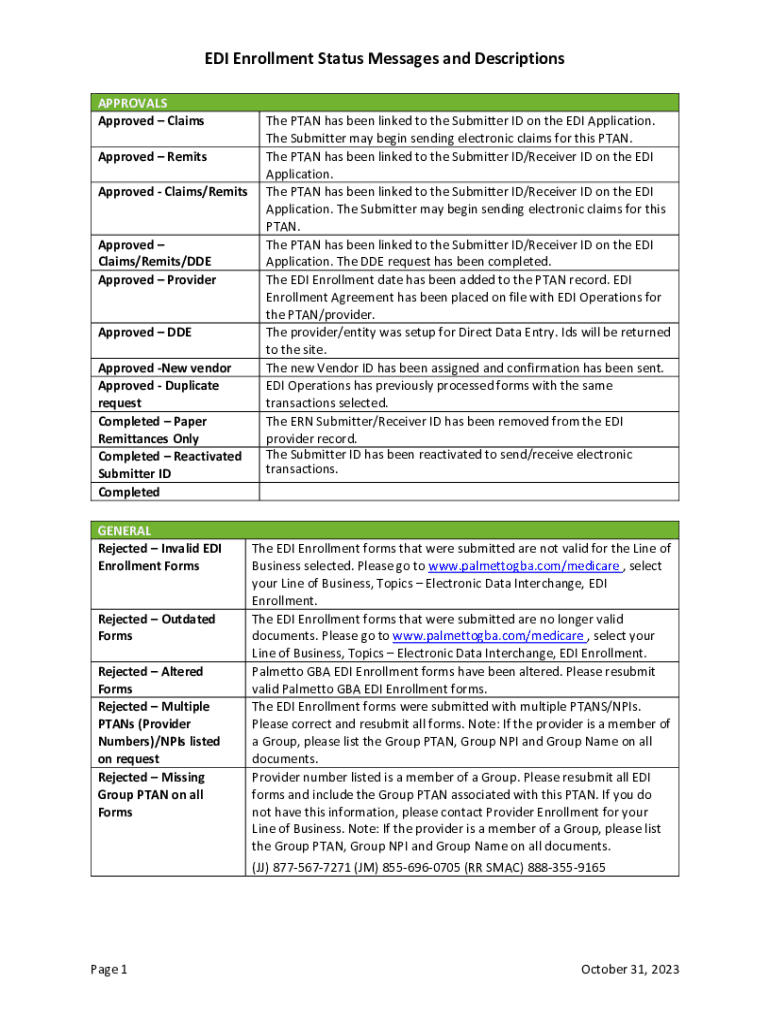
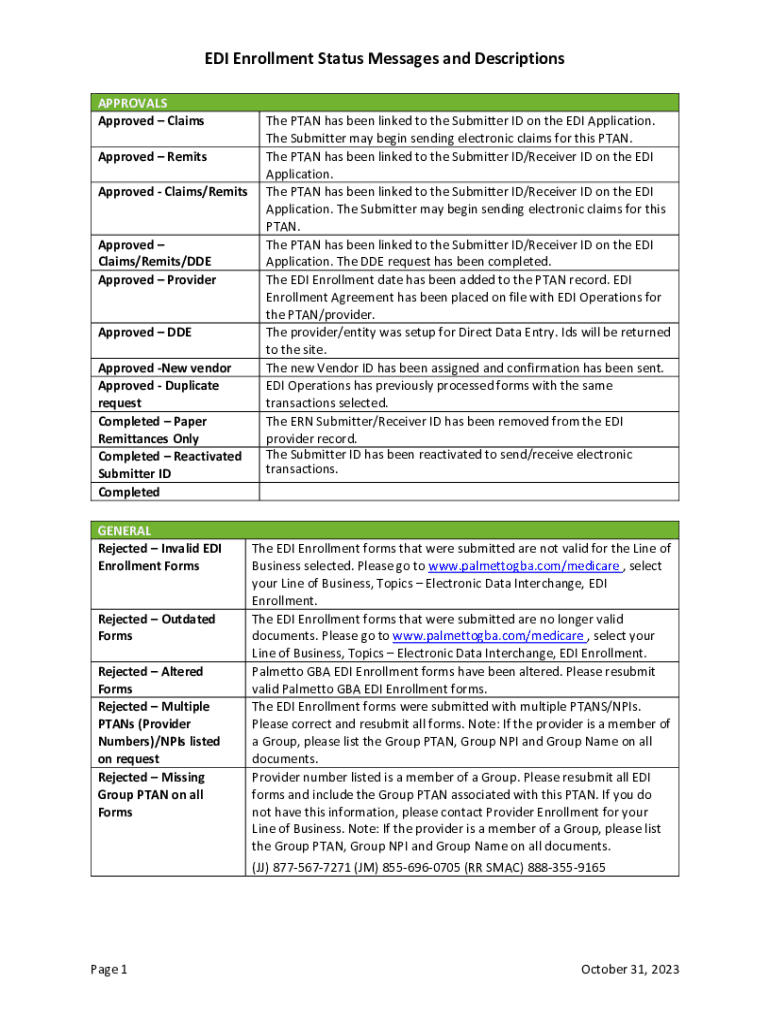
Overview of claims EDI processing
Claims EDI processing refers to the electronic submission and handling of health insurance claims through the Electronic Data Interchange (EDI) system. This method allows healthcare providers to send and receive claims electronically, minimizing manual intervention and paperwork. With the growth of digital solutions in healthcare, EDI has become a critical component in streamlining claims workflows.
The importance of EDI in healthcare and insurance cannot be overstated. It enhances efficiency, reduces claim rejections due to inaccuracies, and accelerates payment cycles, ultimately improving cash flow for providers. Additionally, EDI fosters better communication between payers and providers, facilitating a more effective reimbursement process.
Understanding the 6 claims EDI processing form
The 6 Claims EDI Processing Form is specifically designed to standardize the submission of multiple insurance claims to various payers. Its purpose includes not only facilitating the claims submission but also ensuring that all necessary information is captured according to specific EDI standards. This form is significant as it helps simplify the complexities involved in the often convoluted claims process.
Different types of claims can be processed using the 6 Claims EDI form, including medical, dental, and even specialty claims. To streamline operations, the key stakeholders involved typically include healthcare providers, billing specialists, insurers, and sometimes third-party vendors who assist with claims management.
Steps to complete the 6 claims EDI processing form
Completing the 6 Claims EDI Processing Form involves several essential steps, ensuring that each claim is correctly submitted without issues.
Best practices for using the 6 claims EDI processing form
To maximize the effectiveness of the 6 Claims EDI Processing Form, it’s crucial to adhere to best practices that ensure precision and compliance.
Troubleshooting common issues in EDI claims processing
Navigating electronic claims processing can sometimes lead to common challenges. It’s important to tackle these proactively to avoid delays in payment.
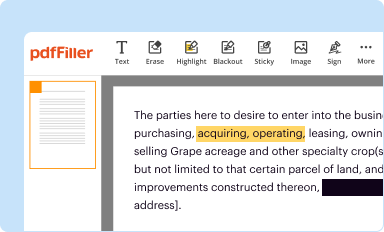
Enhancing collaboration and efficiency with pdfFiller
With numerous stakeholders involved in claims processing, utilizing a platform like pdfFiller significantly enhances collaboration and efficiency. This cloud-based solution allows for seamless teamwork and communication, which is critical in addressing claims quickly.
pdfFiller incorporates features that facilitate engagement among team members. Real-time editing, shared access to documents, and integrated messaging systems help streamline the claims process. Cloud-based document management also ensures that everyone has access to the latest version, eliminating discrepancies.
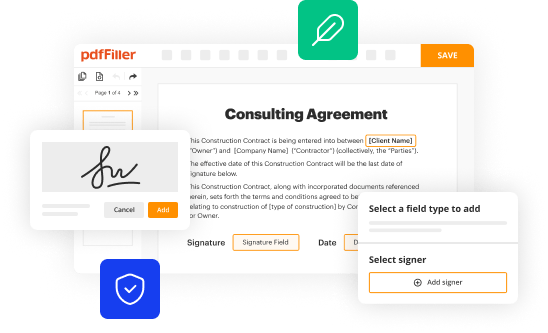
Interactive tools and resources available on pdfFiller
pdfFiller provides a suite of interactive tools that can significantly enhance the experience of completing the 6 Claims EDI Processing Form. The platform offers customizable form templates that allow users to modify documents to fit their specific needs.
Frequently asked questions about the 6 claims EDI processing form
As users engage with the 6 Claims EDI Processing Form, many questions often arise regarding its use and the broader EDI processing framework.
Case studies on successful EDI processing
Numerous healthcare organizations have reported enhanced efficiency and reduced processing times since implementing the 6 Claims EDI Processing Form. By automating claims submissions and utilizing electronic systems, these organizations have seen measurable reductions in claim resolution times, leading to improved cash flow.
For instance, a regional medical facility adopted the EDI process and noted a 30% decrease in claims rejections due to improved accuracy in submissions. This translated to quicker reimbursements from insurance providers, demonstrating the tangible benefits of embracing electronic claims processing.






For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
How can I edit 6 claims edi processing from Google Drive?
How can I get 6 claims edi processing?
How do I edit 6 claims edi processing on an iOS device?
What is 6 claims edi processing?
Who is required to file 6 claims edi processing?
How to fill out 6 claims edi processing?
What is the purpose of 6 claims edi processing?
What information must be reported on 6 claims edi processing?
pdfFiller is an end-to-end solution for managing, creating, and editing documents and forms in the cloud. Save time and hassle by preparing your tax forms online.