Get the free Evaluating Risk Adjustment and Medicare Advantage Ideas for ...
Get, Create, Make and Sign evaluating risk adjustment and
How to edit evaluating risk adjustment and online
Uncompromising security for your PDF editing and eSignature needs
How to fill out evaluating risk adjustment and
How to fill out evaluating risk adjustment and
Who needs evaluating risk adjustment and?
Evaluating Risk Adjustment and Form
Understanding risk adjustment in healthcare
Risk adjustment is a crucial process in healthcare that involves adjusting payments to health plans based on the health status and risk level of enrolled patients. This method ensures that providers who care for higher-risk populations receive appropriate compensation. Without risk adjustment, healthcare systems could face inequities, as payers might be incentivized to enroll healthier patients. The overall objective is to create a fairer financial landscape that accurately reflects the care requirements of different patient populations.
The importance of risk adjustment in healthcare cost management cannot be overstated. By evaluating the risk associated with patient populations, healthcare organizations can allocate resources more effectively and manage overall expenses. As insurers calculate reimbursement rates, including risk scores derived from medical records, it becomes essential for healthcare providers to deliver comprehensive documentation that reflects the severity of their patients' conditions.
Your role in the risk adjustment process
To effectively navigate the risk adjustment landscape, it's crucial to identify and understand your role within the process. Providers, coders, and administrators each play unique yet interconnected roles. Healthcare providers must focus on delivering high-quality care while documenting that care comprehensively. Coders are responsible for translating clinical narratives into accurate codes that will affect reimbursement rates. Administrators manage policies and workflows that facilitate effective risk adjustment.
Accurate documentation and coding are essential responsibilities of each role. A provider must articulate a patient’s medical condition and treatment thoroughly, allowing coders to select correct codes that reflect the patient’s health status. Coder error can lead to inadequate reimbursement or compliance issues, making collaboration among teams vital for success. Establishing an open line of communication ensures all team members are aligned on the importance of risk adjustment.
The foundation of risk adjustment: medical record requirements
A well-maintained medical record serves as the backbone of the risk adjustment process. Essential elements include comprehensive patient demographics, a detailed problem list, treatment history, and current medications. Each component must align with documentation standards that detail patient interactions, diagnoses, and any prescribed treatments. This extensive information is crucial when health plans evaluate risk scores for reimbursement.
Documenting all relevant details in patient medical records is non-negotiable. Inadequate documentation could have severe consequences, such as delayed reimbursements or inaccurate risk scores leading to financial penalties. Providers must ensure that their records are up-to-date and meet the required documentation standards set forth by governing healthcare organizations.
Important coding and medical record documentation information
Coding relevance cannot be overstated in the context of risk adjustment. The industry primarily utilizes coding systems such as ICD (International Classification of Diseases), CPT (Current Procedural Terminology), and HCPCS (Healthcare Common Procedure Coding System) to represent patient diagnoses and services rendered. These codes significantly influence the risk adjustment process as they directly affect risk scores and ultimately reimbursement rates.
Common coding errors to avoid include selecting the wrong codes, failing to document all pertinent information, and neglecting updates in coding standards. Moreover, correct application can involve understanding the nuances of each coding system. Institutions must prioritize training for coding professionals, ensuring they are adept at identifying proper codes reflective of documented conditions, especially for chronic patients who often have multiple health issues.
Guidelines for chronic condition management in risk adjustment
Chronic conditions such as diabetes, hypertension, and heart disease necessitate particular attention within the risk adjustment framework. These conditions profoundly influence risk scores and, by extension, reimbursement rates. Identifying chronic conditions accurately requires comprehensive documentation and understanding of their implications for patient care and the reimbursement process.
Effective documentation techniques for chronic conditions can include the use of standardized assessments and regular monitoring of patient progress. Moreover, techniques for patient engagement can significantly impact adherence to treatment plans. Educating patients about their conditions fosters cooperation and leads to more accurate and consistent data collection, essential for successful risk adjustment initiatives.
Evaluating the effectiveness of risk adjustment initiatives
Assessing the success of risk adjustment initiatives requires a clear understanding of metrics. Key performance indicators (KPIs) may include reduction in claim denials, improved patient outcomes, and enhanced reimbursement accuracy. By analyzing these metrics, healthcare organizations can determine whether their risk adjustment processes are functioning optimally.
Tools for analyzing risk adjustment data range from specialized analytics software to management dashboards. These tools help organizations visualize trends over time, enabling informed decision-making. Case studies of successful risk adjustment implementations illustrate the potential benefits of adopting robust monitoring practices, ultimately leading to lasting improvements in healthcare quality and cost-efficiency.
Interactive tools for risk adjustment evaluation
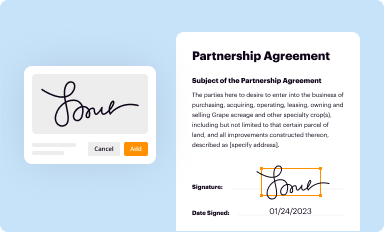
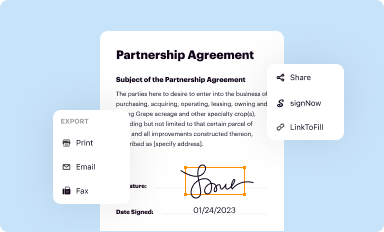
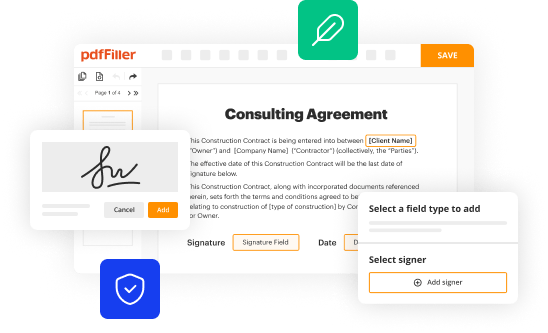
Interactive tools, such as those offered by pdfFiller, play a vital role in effectively managing documents related to risk adjustment. These solutions allow healthcare teams to create, edit, and collaborate on documents anywhere, improving the efficiency of the risk adjustment process. They can streamline workflows, reduce errors, and enhance communication among stakeholders.
Utilizing interactive tools involves a step-by-step approach, including setting up forms to capture patient data accurately and securely. With integrated e-signature capabilities, healthcare professionals can easily obtain the necessary approvals, thus creating a smooth documentation flow. The benefits of employing digital solutions extend beyond convenience, as they also enhance compliance with documentation standards critical in risk adjustment.
Resources for continuous improvement in risk adjustment
Continuous improvement in risk adjustment practices is paramount as healthcare paradigms shift. Engaging with industry guidelines, including those from leading organizations such as the American Health Information Management Association (AHIMA) or the Centers for Medicare and Medicaid Services (CMS), provides healthcare organizations with current best practices. Regular training sessions and workshops enhance the capabilities of the involved workforce.
Furthermore, investing in recommended reading can support ongoing education, while participation in professional organizations creates networking opportunities for sharing insights. Access to the latest developments ensures that organizations remain abreast of the changes that impact risk adjustment, allowing them to adapt proactively.
Navigating changes: updates on coverage and reimbursement
Current trends in risk adjustment significantly impact reimbursement structures. Ongoing legislative changes and healthcare reforms demand that organizations stay informed about how policy shifts affect coding and claim submissions. Providers must remain agile, prepared to adapt to changes that could alter reimbursement rates based on evolving risk assessment methodologies.
Recent revisions affecting coding practices require healthcare teams to review protocols regularly. Staying updated can prevent missed opportunities for proper reimbursements and assist in maximizing efficiency in risk adjustment processes. Preparing for future changes provides organizations a competitive edge in navigating the dynamic landscape of healthcare finance.
Frequently asked questions about risk adjustment
There are many common concerns and misconceptions surrounding risk adjustment. Addressing inquiries not only demystifies the process for stakeholders but also enhances overall compliance. Engaging in discussions to clarify complex topics such as coding nuances or documentation requirements encourages better understanding and cooperation among teams.
Staying informed on developments in risk adjustment practices can be a challenge, particularly with constant changes. Regularly reviewing updates from authoritative sources equips healthcare organizations with the knowledge needed to navigate complexities, ensuring they maintain compliance and improve their documentation processes.






For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
How can I edit evaluating risk adjustment and from Google Drive?
Can I create an eSignature for the evaluating risk adjustment and in Gmail?
How do I complete evaluating risk adjustment and on an Android device?
What is evaluating risk adjustment?
Who is required to file evaluating risk adjustment?
How to fill out evaluating risk adjustment?
What is the purpose of evaluating risk adjustment?
What information must be reported on evaluating risk adjustment?
pdfFiller is an end-to-end solution for managing, creating, and editing documents and forms in the cloud. Save time and hassle by preparing your tax forms online.