Get the free Prior Authorization Repetitive Scheduled Non-Emergent ...
Get, Create, Make and Sign prior authorization repetitive scheduled



How to edit prior authorization repetitive scheduled online
Uncompromising security for your PDF editing and eSignature needs
How to fill out prior authorization repetitive scheduled

How to fill out prior authorization repetitive scheduled
Who needs prior authorization repetitive scheduled?
Understanding the Prior Authorization Repetitive Scheduled Form
Understanding prior authorization in healthcare
Prior authorization is a crucial tool in healthcare management designed to control costs and ensure that patients receive appropriate care based on medical necessity. It is a requirement from health insurance companies, mandating providers to obtain approval for certain services or medications before they can be covered. This process helps insurers manage patient care costs and ensures that procedures align with evidence-based guidelines.
The importance of prior authorization cannot be understated. It safeguards against unnecessary treatments and expenses, ultimately promoting efficient healthcare resource utilization. Many services, particularly high-cost ones, often demand prior authorization to prevent misuse of health insurance resources, which helps lower premiums and maintain overall healthcare affordability.
Services that typically require prior authorization include specialized surgeries, high-cost medications, and diagnostic imaging. Healthcare providers must navigate this framework effectively to provide timely care for their patients.
Prior authorization for repetitive scheduled services
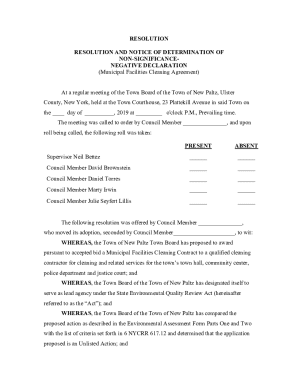
Repetitive scheduled non-emergent services consist of routine procedures or treatments that patients require regularly, which necessitates prior authorization for ongoing coverage. These can involve a variety of healthcare applications, primarily when they involve equipment or transport that must be scheduled in advance.
Common scenarios that require prior authorization include repetitive medical equipment such as wheelchairs or nebulizers, scheduled therapy services like physical or occupational therapy, and non-emergent ambulance transport for routine clinic visits. Addressing the details involved in these cases is critical to ensuring efficient patient care.
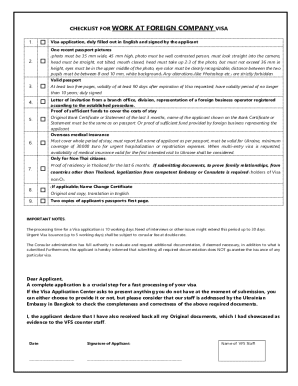
The prior authorization process
Understanding the prior authorization process is vital for healthcare providers and patients alike. The following steps provide a clear guide to navigating this sometimes intricate process effectively.
To ensure a smooth submission process, always double-check that all required fields are filled out correctly, and criteria are met. Familiarity with the specifics of the insurance provider's requirements can save valuable time.
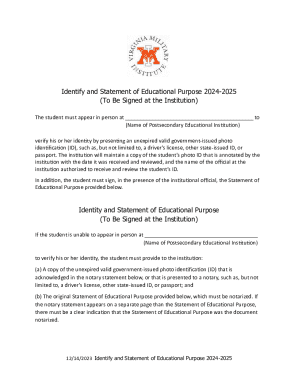
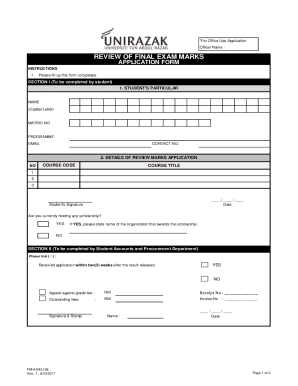
Required information for completing the form
Filling out the prior authorization repetitive scheduled form requires meticulous attention to detail, ensuring that no essential information is overlooked. The essential patient information typically includes full name, date of birth, insurance details, and diagnosis codes.
Details about the requested service should outline the specific procedure or equipment needed, specifying frequency and duration. Additionally, supporting documentation may also be necessary, including physician notes, imaging results, and the corresponding HCPCS codes for services requested, which further clarify the medical necessity of the authorization.
Interactive tools for managing prior authorizations on pdfFiller
pdfFiller equips healthcare providers and patients with interactive tools that simplify the management of prior authorizations. By leveraging a cloud-based document management system, users can easily handle forms such as the prior authorization repetitive scheduled form without the hassle of physical paperwork.
One of the key features includes eSignature capabilities, which streamline the process of signing forms remotely. Furthermore, collaborative editing allows multiple parties to work on the same document, improving efficiency and avoid discrepancies.
Users can upload and edit forms seamlessly, allowing for quick adjustments as needed. The intuitive interface makes the process straightforward, ensuring that interactive tools foster efficient submission and approval workflows.
Common challenges and solutions in prior authorization
The prior authorization process, while necessary, can present various challenges that healthcare providers must navigate. Common delays in approval often stem from incomplete submissions or miscommunication with insurers. Understanding these challenges can aid providers in overcoming them effectively.
A proactive approach is essential in avoiding missing information. Providers should create checklists and guidelines based on insurer-specific requirements to streamline the submission process. In case of denials, it's crucial to understand the appeal process and gather sufficient documentation to support the appeal.
Providing a straightforward appeal process overview and suggested documentation needed can empower providers to advocate effectively for their patients.
Best practices for healthcare providers and patients
Adhering to best practices in the prior authorization workflow can significantly improve patient care while reducing unnecessary delays. For providers, ensuring timely submissions is essential for maintaining patient satisfaction and continuity of care.
For patients, preparing a checklist of necessary documents before appointments can save time and frustration. Additionally, keeping track of authorization expiration dates ensures that patients don’t encounter abrupt service interruptions.
Navigating repetitive scheduled non-emergent ambulance transport
Non-emergent ambulance transport has specific guidelines that must be followed to ensure that prior authorization is processed smoothly. Unlike emergency services, these transports require documented medical necessity to warrant coverage.
The relevant HCPCS codes facilitate appropriate billing but also play an essential role in justifying the need for such transport. It's vital for providers to be aware of the case scenarios that justify the use of a non-emergent ambulance, ensuring that patients have access to a beneficial service without unnecessary financial strain.
Providers should always be prepared with comprehensive documentation and reasoning to support the need for such services.
Utilizing pdfFiller for ongoing document management
Utilizing pdfFiller for managing documents optimizes workflows in healthcare settings. Its cloud-based platform offers numerous benefits, allowing users to access necessary forms at their convenience, facilitating prompt submissions and responsive patient care.
Collaboration among healthcare teams is enhanced through pdfFiller, ensuring that all parties can work on the same document, significantly reducing the chances of errors or missed information. The ability to access documents from any device promotes flexibility, making it easier to manage and share documentation effectively.
Frequently asked questions (FAQs)
Understanding common queries related to the prior authorization repetitive scheduled form enhances knowledge in navigating the process. When authorization is denied, providers can reapply or appeal the decision with additional supporting information.
Timelines for approval vary, but it’s essential to follow up regularly to expedite answers. If new information arises, resubmission is possible and can often lead to a different outcome, showcasing the importance of collaboration and communication between providers and insurers.






For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
Can I create an eSignature for the prior authorization repetitive scheduled in Gmail?
How do I edit prior authorization repetitive scheduled straight from my smartphone?
How can I fill out prior authorization repetitive scheduled on an iOS device?
What is prior authorization repetitive scheduled?
Who is required to file prior authorization repetitive scheduled?
How to fill out prior authorization repetitive scheduled?
What is the purpose of prior authorization repetitive scheduled?
What information must be reported on prior authorization repetitive scheduled?
pdfFiller is an end-to-end solution for managing, creating, and editing documents and forms in the cloud. Save time and hassle by preparing your tax forms online.