Get the free Pharmacy Request for Prior Approval FormSaphnelo - Providers - AmeriHealth Caritas N...
Get, Create, Make and Sign pharmacy request for prior



How to edit pharmacy request for prior online
Uncompromising security for your PDF editing and eSignature needs
How to fill out pharmacy request for prior

How to fill out pharmacy request for prior
Who needs pharmacy request for prior?
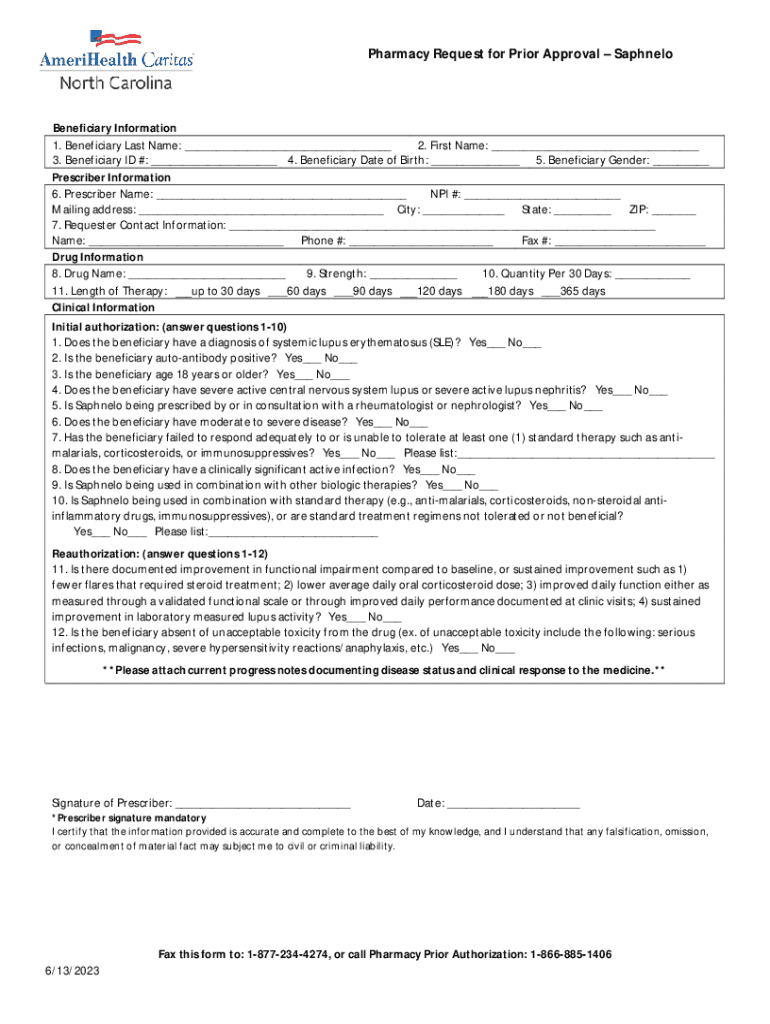
Pharmacy Request for Prior Form: A Comprehensive Guide
Understanding pharmacy prior authorization
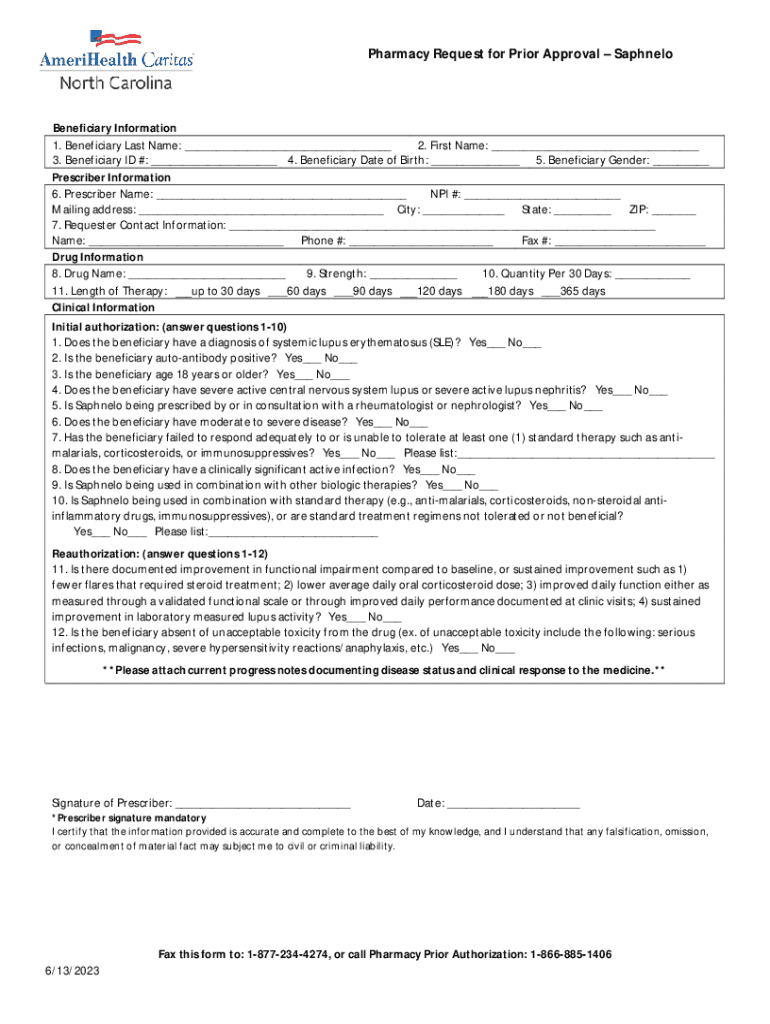
Pharmacy prior authorization (PA) is a crucial process whereby health insurance companies review requests for certain medications before they are prescribed to patients. This approval must be obtained prior to purchasing specific medications and is essential for ensuring that each prescription aligns with the patient’s health needs and the insurer's policies. The importance of prior authorization lies not only in controlling healthcare costs but also in enabling healthcare providers to prescribe medications that reflect best practices in patient care.
Numerous medications, particularly those categorized as high-cost, specialty drugs, or those associated with potential misuse, often require a pharmacy prior authorization. Common examples include medications for chronic conditions such as rheumatoid arthritis, cancer treatments, and medications that may not be first-line therapies.
The pharmacy request for prior form
The pharmacy request for prior form is an essential document that patients and healthcare providers need to complete to initiate the authorization process. This form collects pertinent information necessary for the insurance company to evaluate the request. Understanding its main components can significantly influence the efficiency of the submission and eventual approval.
Steps to complete the pharmacy request for prior form
Completing the pharmacy request for prior form involves a systematic approach aimed at minimizing errors and expediting the authorization process.
Submitting the pharmacy request for prior form
After successfully filling out the pharmacy request for prior form, the next step is to submit it. The method of submission can significantly affect the speed of the authorization process.
Generally, the response to the authorization request can take anywhere from a few hours to several business days. Delays in authorization can occur for various reasons, such as incomplete information or the need for additional clinical documentation.
Managing your pharmacy prior authorization request
Once the pharmacy request for prior form is submitted, managing its status becomes pivotal for the patient's pharmaceutical care. Patients and providers must know how to follow up effectively.
Related forms and publications
Understanding pharmacy prior authorization does not stop at the initial request. Several related forms and publications can aid patients and providers in navigating this complex process.
Connect with us
For additional assistance concerning the pharmacy request for prior form, pdfFiller offers a range of support options for users needing help.
For immediate assistance, an online chat feature is available, allowing users to connect with customer service representatives quickly.
Quick links
Direct access to essential resources can significantly ease the process of managing the pharmacy request for prior form.






For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
Where do I find pharmacy request for prior?
Can I create an electronic signature for the pharmacy request for prior in Chrome?
How can I edit pharmacy request for prior on a smartphone?
What is pharmacy request for prior?
Who is required to file pharmacy request for prior?
How to fill out pharmacy request for prior?
What is the purpose of pharmacy request for prior?
What information must be reported on pharmacy request for prior?
pdfFiller is an end-to-end solution for managing, creating, and editing documents and forms in the cloud. Save time and hassle by preparing your tax forms online.