Get the free ajovy prescription and service request form
Get, Create, Make and Sign ajovy prescription and service



Editing ajovy prescription and service online
Uncompromising security for your PDF editing and eSignature needs
How to fill out ajovy prescription and service

How to fill out ajovy prior authorization request
Who needs ajovy prior authorization request?
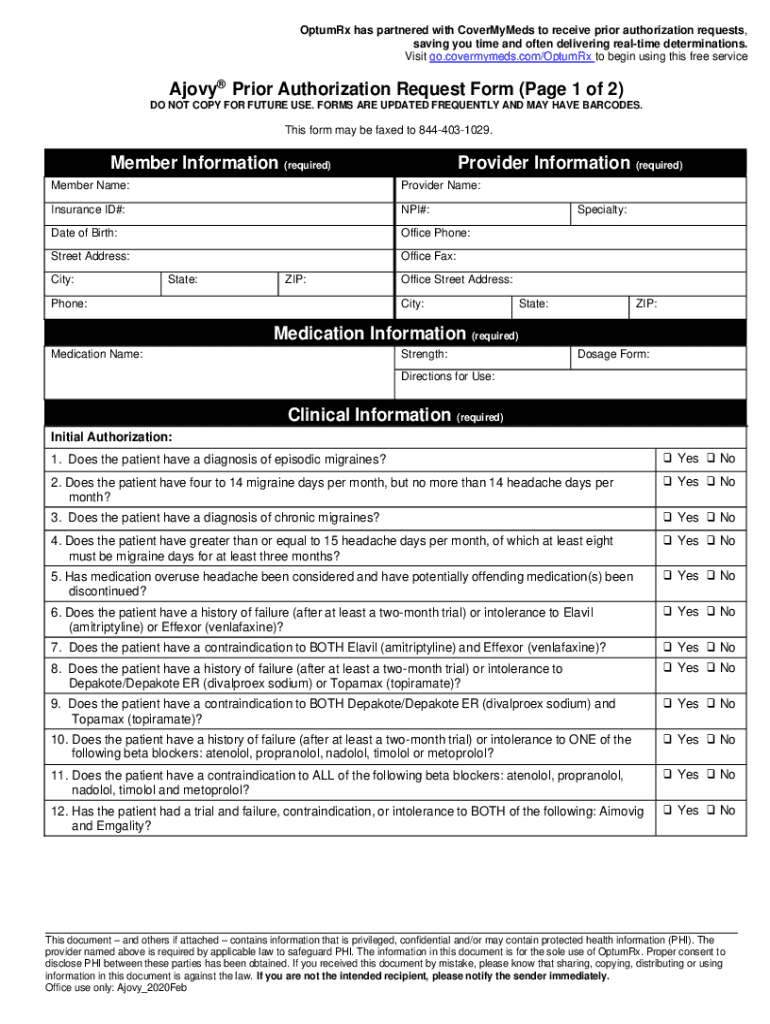
A comprehensive guide to the Ajovy prior authorization request form
Understanding prior authorization for Ajovy
Prior authorization is a requirement by health insurance companies that certain services or medications be approved before they are provided to the patient. This process ensures that the proposed treatment is medically necessary and covered under the patient's insurance plan. Ajovy, a medication used in the prevention of migraines, often necessitates this prior authorization due to its high costs and specialized use.
Recognizing the role of Ajovy in migraine prevention is essential. For individuals who suffer from chronic migraines, Ajovy offers a viable option, but gaining access involves navigating the obstacles of insurance requirements. Prior authorization helps ensure that patients receive the most effective treatment tailored to their health circumstances, but it can also lead to confusion and stress.
Why you need to fill out the Ajovy request form
Filling out the Ajovy prior authorization request form is not just a bureaucratic step; it's a crucial procedure for obtaining coverage from insurance providers. Without this authorization, patients may face substantial out-of-pocket costs or even be denied essential treatment altogether.
The importance of obtaining this coverage cannot be overstated. Ajovy can cost upwards of $6,000 per year without insurance coverage, making the financial implications of not securing prior authorization significant. Given the high price tag, filling out the request form could mean the difference between receiving necessary care or struggling to afford treatment.
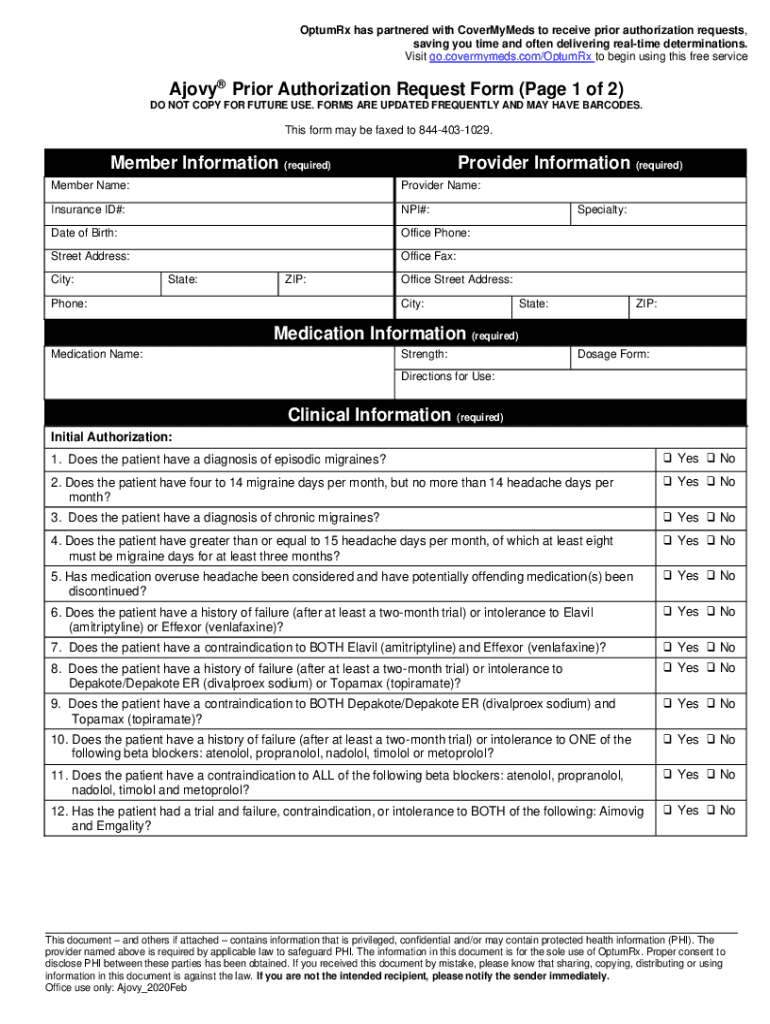
Essential information required for the Ajovy prior authorization request form
To successfully complete the Ajovy prior authorization request form, specific pieces of information are required. These include comprehensive details about the patient, medication history, and the current health condition.
Step-by-step guide to completing the Ajovy prior authorization request form
Completing the Ajovy prior authorization request form can be a daunting process. However, following a structured approach can simplify it significantly.
Submitting the Ajovy prior authorization request form
Once the Ajovy prior authorization request form is filled out, the next step is submission. There's a range of methods to do this, including mail, fax, or online submission via your insurance provider's system. Each insurance provider may have different guidelines, so adhering to these is critical.
After submission, it is important to follow up. Confirm receipt of the request and inquire about the status of the authorization to ensure that the process is moving forward.
What to expect after submission
After submitting the Ajovy prior authorization request form, patients can typically expect a waiting period before receiving a decision. This timeline can vary based on the insurance provider and the complexity of the case, but it usually ranges from a few days to a couple of weeks.
It's crucial to understand the appeals process in case of a denied authorization. Insurance providers are required to explain why a request was denied, providing the opportunity to rectify issues or present additional information to support the request.
Utilizing pdfFiller for the Ajovy request form
pdfFiller offers an innovative solution for managing the Ajovy prior authorization request form. By utilizing pdfFiller, users can enjoy a seamless experience from editing to submission.
Common challenges and frequently asked questions
Navigating the prior authorization process typically comes with its set of challenges. Many patients express concern over the complexity of the forms, the length of time required for decisions, and issues related to insufficient information.
Common questions include inquiries about how long the authorization process takes and what to do if the request is denied. Understanding these challenges can empower patients, allowing them to better prepare for the submission process and facilitate communication with their healthcare providers.
Additional tips for a successful prior authorization process
To ensure a smooth experience, consider adopting some best practices during the prior authorization process.






For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
How can I get ajovy prescription and service?
How do I edit ajovy prescription and service straight from my smartphone?
How do I fill out ajovy prescription and service on an Android device?
What is ajovy prior authorization request?
Who is required to file ajovy prior authorization request?
How to fill out ajovy prior authorization request?
What is the purpose of ajovy prior authorization request?
What information must be reported on ajovy prior authorization request?
pdfFiller is an end-to-end solution for managing, creating, and editing documents and forms in the cloud. Save time and hassle by preparing your tax forms online.