Get the free ajovy patient assistance form pdf
Get, Create, Make and Sign ajovy shared solutions form



Editing ajovy patient assistance form online
Uncompromising security for your PDF editing and eSignature needs
How to fill out ajovy patient assistance form

How to fill out ajovy fremanezumab-vfrm prior authorization
Who needs ajovy fremanezumab-vfrm prior authorization?
Ajovy fremanezumab-vfrm prior authorization form: A comprehensive guide
Understanding Ajovy and its applications
Ajovy, also known by its generic name fremanezumab, is a groundbreaking medication designed specifically for the prevention of migraines. Administered once a month or quarterly, Ajovy functions by inhibiting the activity of calcitonin gene-related peptide (CGRP), a molecule implicated in migraine development. This targeted approach can significantly reduce the frequency of migraine attacks in patients suffering from chronic and episodic migraines, making it a vital option for those with debilitating conditions.
The efficacy of Ajovy has been supported by clinical trials, showing substantial improvement in patients’ quality of life through fewer migraine days each month. However, it is crucial to understand that while Ajovy offers a promising solution for migraine sufferers, it is not intended for the acute treatment of migraines once they occur.
Important safety information
While Ajovy is beneficial for many, it is essential to consider some important safety information. Adverse reactions may include injection site reactions, constipation, and hypersensitivity reactions. Patients with a history of such reactions or those who are pregnant or breastfeeding should consult their healthcare provider before starting treatment. Knowing these considerations ensures informed decision-making for patients and their doctors.
Why prior authorization is necessary
Prior authorization is a cost-control mechanism used by health insurance companies to determine the medical necessity of prescribed treatments. It ensures that before the medication is prescribed, the insurance will review the request to ensure that it is justified according to their criteria. This process is particularly important for high-cost medications like Ajovy, where insurers need to verify that patients have met specific clinical guidelines.
The importance of prior authorization extends to ensuring that patients only receive treatments that are deemed appropriate and effective based on their medical history. This additional step can help manage healthcare costs by ensuring that only those who truly require the medication receive it. Additionally, the process can sometimes help identify alternative, lower-cost options that may also be effective.
Common insurance requirements
Many insurance providers have established specific requirements for the prior authorization of Ajovy. Typically, these requirements can vary but often include documentation showing the patient's diagnosis of migraine, confirmation of prior treatments attempted, and evidence that assert the patient meets the clinical criteria outlined by the insurance company. Understanding these requirements is crucial for a smooth approval process.
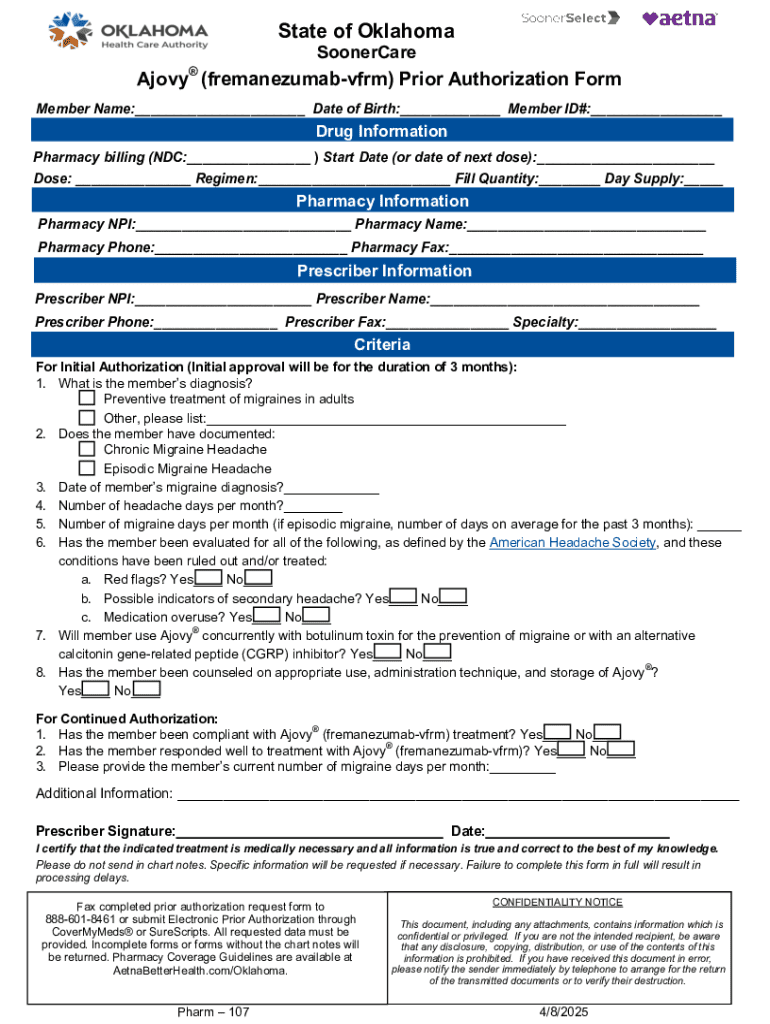
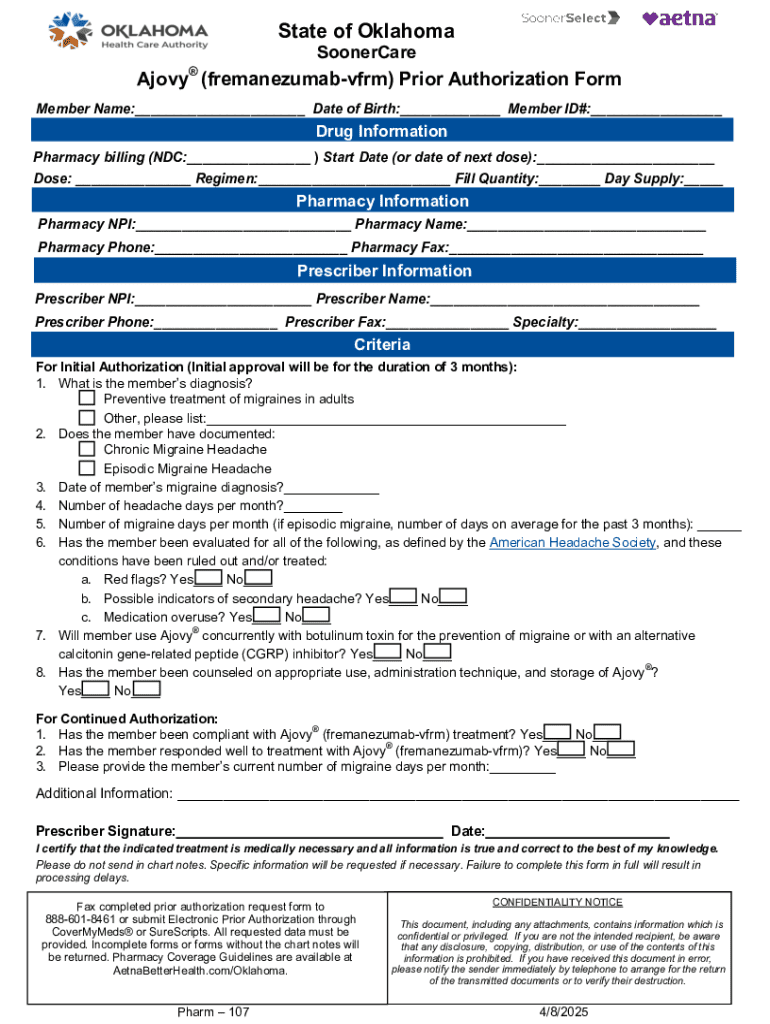
Overview of the prior authorization form for Ajovy
The Ajovy prior authorization form is a pivotal document that allows healthcare providers to request approval from insurance companies for the medication. This form plays a significant role in delineating why Ajovy is necessary for the patient's treatment plan. Completing this form accurately is critical, as it directly influences the approval process.
Professionals must pay attention to key sections of the form, including patient demographics, diagnosis, previous treatment attempts, and specific justifications for the use of Ajovy. Forms that lack sufficient detail or fail to provide a compelling rationale may face denial.
Step-by-step instructions for completing the Ajovy prior authorization form
Completing the Ajovy prior authorization form can be straightforward with proper preparation. First, gather necessary patient information, including the patient’s full name, insurance details, and contact information. It is also essential to compile any relevant medical history, which will assist in supporting the application.
After gathering documents, move into filling out the different sections of the form.
Preparation steps
Filling out the form
Before submission, review and double-check all entries. Look out for common mistakes such as incorrect patient details or missed sections, which could lead to delays or denials.
Submitting the Ajovy prior authorization form
Once completed, the next step is to submit the Ajovy prior authorization form. Insurance providers will typically have different submission methods—these may include online portals, faxing, or mailing the form. It is important to refer to your specific insurance provider’s guidelines to ensure proper submission for efficient processing.
Following up on the status of your prior authorization is crucial. Contact the insurance company within 5-7 business days after submission to check if the request has been received and processed. This proactive approach can assist in identifying any issues early in the process. Keep documentation of all communication for reference.
Follow-up procedures
Managing the approval process
Understanding the criteria that insurers look for in approving a prior authorization for Ajovy can be extremely beneficial. Commonly, insurance companies will examine the documentation of the patient's medical history, previous treatment failures, and the potential for Ajovy to significantly enhance the patient's quality of life. Being thorough in the prior authorization application process is essential to overcome any potential obstacles.
However, despite best efforts, denials can occur. It is crucial to know how to address such situations. Common reasons for denials include inadequate documentation, insufficient treatment history, or a lack of evidence for medical necessity.
Addressing denials
Utilizing pdfFiller for enhanced document management
pdfFiller is an invaluable resource for managing the Ajovy fremanezumab-vfrm prior authorization form. Its cloud-based platform allows users to seamlessly edit PDFs, complete the authorization form online, and utilize eSigning capabilities for quick and verified approvals. This ensures you have a secure and efficient way to handle the form while minimizing the potential for delays.
Using pdfFiller can enhance your overall document management experience significantly. The ability to store and retrieve documents from anywhere means that both healthcare providers and patients can easily keep track of all necessary paperwork, which is key in the fast-paced world of healthcare.
Step-by-step: Editing the Ajovy form on pdfFiller
Editing the Ajovy prior authorization form using pdfFiller is straightforward. Begin by uploading your form into the platform. You can easily edit all text fields, add necessary annotations, and ensure that all information is accurate before submission.
Interactive tools available on pdfFiller
In addition to editing and eSign features, pdfFiller provides robust collaborative options. Users can invite team members or healthcare providers to contribute to the document, ensuring everyone involved has access to the most up-to-date information.
Furthermore, tracking changes in documents enhances the transparency of the approval process. Having records of who made changes and when can be invaluable should disputes or questions arise during the submission and approval of the Ajovy prior authorization form.
Final considerations for patients and healthcare providers
For patients and healthcare providers alike, understanding the intricacies of the Ajovy fremanezumab-vfrm prior authorization form is essential. Best practices include meticulously gathering all required documentation, providing complete treatment histories, and continuously communicating with insurance providers throughout the process.
Healthcare providers play a crucial role in navigating this process, offering guidance and ensuring that all necessary information is included in the prior authorization request. Their expertise not only streamlines the submission process but also maximizes the chances of approval, ultimately benefiting the patient’s healthcare journey.






For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
How can I modify ajovy patient assistance form without leaving Google Drive?
How can I edit ajovy patient assistance form on a smartphone?
Can I edit ajovy patient assistance form on an Android device?
What is ajovy fremanezumab-vfrm prior authorization?
Who is required to file ajovy fremanezumab-vfrm prior authorization?
How to fill out ajovy fremanezumab-vfrm prior authorization?
What is the purpose of ajovy fremanezumab-vfrm prior authorization?
What information must be reported on ajovy fremanezumab-vfrm prior authorization?
pdfFiller is an end-to-end solution for managing, creating, and editing documents and forms in the cloud. Save time and hassle by preparing your tax forms online.