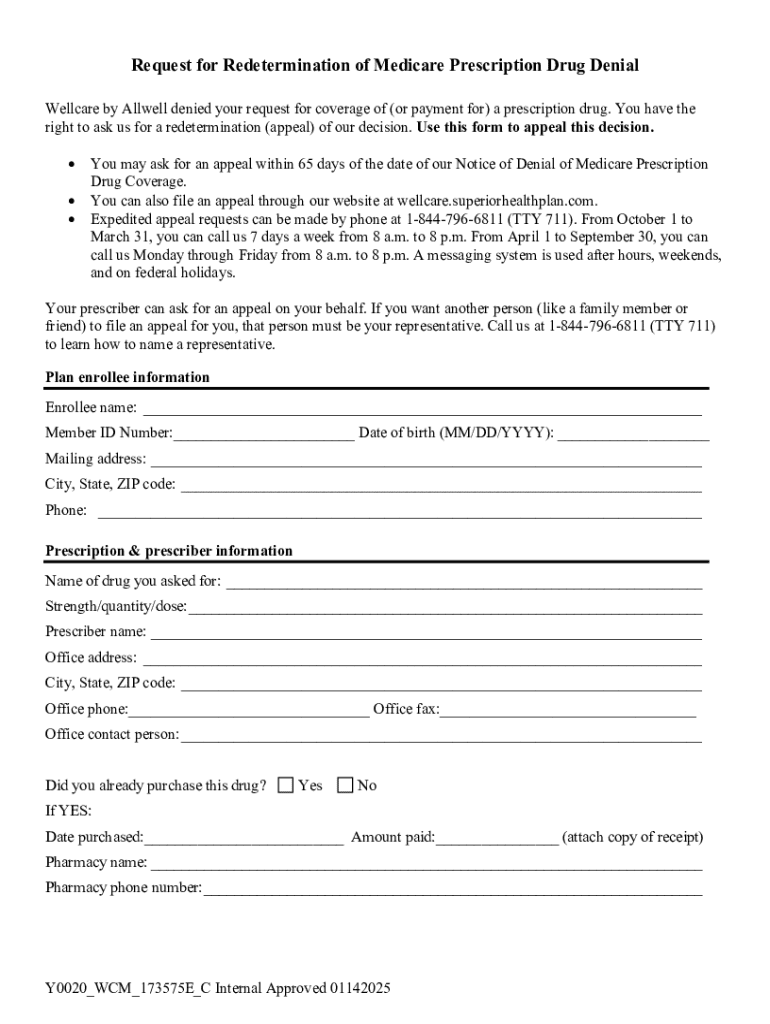
Get the free Coverage Determination Appeal
Get, Create, Make and Sign coverage determination appeal



How to edit coverage determination appeal online
Uncompromising security for your PDF editing and eSignature needs
How to fill out coverage determination appeal

How to fill out coverage determination appeal
Who needs coverage determination appeal?
Coverage Determination Appeal Form: How-to Guide
Understanding the coverage determination appeal process
Coverage determination appeals are a critical component of healthcare management, enabling individuals and providers to contest decisions made by insurance companies regarding coverage. Understanding this process is crucial for anyone navigating the often complex healthcare system.
A coverage determination appeal occurs when a healthcare service or product is denied coverage by a health insurance provider. This process allows patients to assert their rights and request that a denial be re-evaluated based on evidence and insist that their case be reviewed thoroughly.
Who should use the coverage determination appeal form?
The coverage determination appeal form can be beneficial to both individuals and teams. Individuals might find themselves in situations where health-related services or medications crucial for their wellbeing are denied. In contrast, healthcare teams, including healthcare advocates and providers, often assist patients in navigating complex appeal processes.
Common scenarios that necessitate an appeal include receiving a letter indicating a service was denied, requiring a medication that has been deemed non-covered, or encountering problems with prior authorization. Knowing when and how to apply for an appeal is crucial for success.
Navigating the coverage determination appeal form
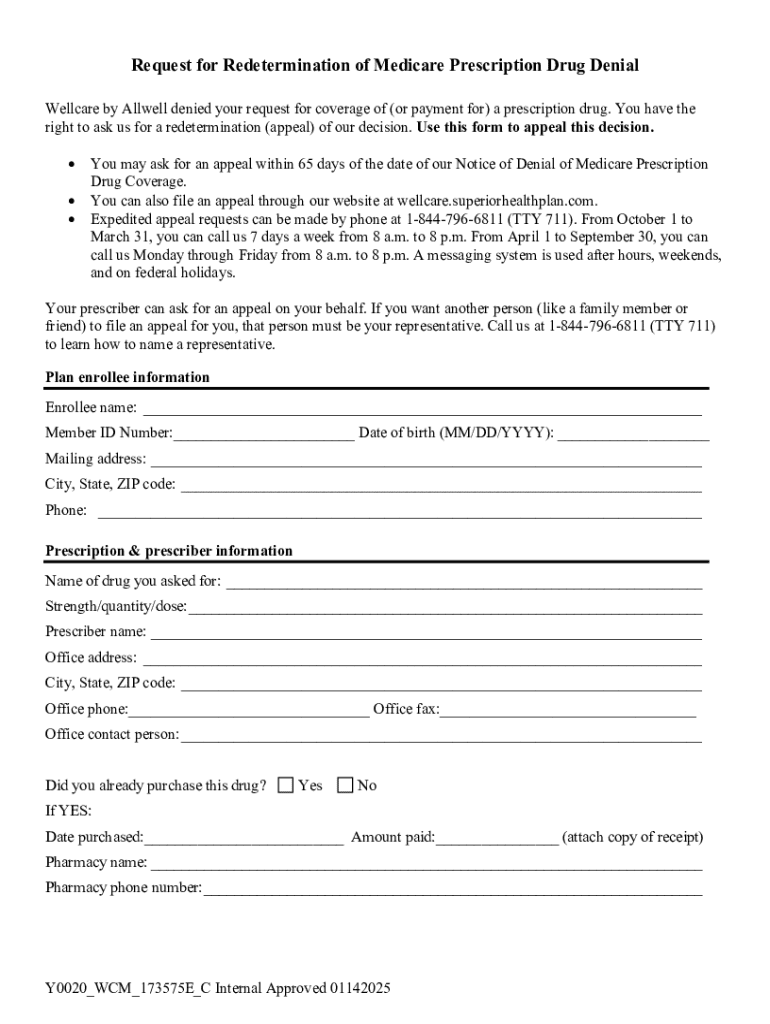
The coverage determination appeal form is structured to facilitate the submission of necessary information in an organized manner. Its primary purpose is to allow patients or their representatives to communicate the specifics of their appeal compellingly.
The form typically includes sections for personal information, details of the coverage in question, and your rationale for contesting the denial. It works seamlessly with other documents, such as supporting evidence and medical records, to present a comprehensive case.
Filling out the coverage determination appeal form
Completing the coverage determination appeal form requires attention to detail, particularly in sections where your personal and coverage information is documented. Ensuring that all provided information is accurate is paramount; errors can lead to delays or outright denials of your appeal.
Specificity is key in the coverage details section. Clearly state the services or items that were denied and provide any relevant identification numbers or claim references. Articulating your reasons for appeal is similarly vital; this is your opportunity to present a compelling case.
Providing strong supporting evidence can dramatically enhance the effectiveness of your appeal. Collect relevant documentation, such as medical records, prescriptions, and letters from healthcare providers that can support your claim.
When presenting your case, be concise. Use bullet points where necessary and avoid lengthy explanations; the goal is to present compelling arguments straightforwardly.
Editing and customizing your appeal form
pdfFiller provides robust editing tools to customize your coverage determination appeal form. Whether you need to fill out the form digitally or adjust sections to suit your needs, pdfFiller's platform offers user-friendly options for modification.
Additionally, collaboration tools can facilitate teamwork when filling out the appeal. If you are working alongside healthcare providers or family members, sharing the document quickly fosters effective communication and ensures that no vital information is overlooked.
Submitting your coverage determination appeal
Once you have completed and edited your appeal form, it's time to submit it. Utilizing pdfFiller's platform simplifies this process significantly. Follow clear step-by-step instructions available on the platform to ensure your submission is done correctly.
If you choose alternative submission methods, such as emailing or mailing a hard copy to your insurance provider, it's essential to understand each option's requirements. Double-check their submission guidelines to avoid complications.
What to expect after submission
After submitting your coverage determination appeal, it’s important to understand the review timeline. Most insurers will aim to provide a decision within 30 days. However, depending on the complexity of your case and the specifics of your insurance policy, this could be longer.
Following up on your appeal is crucial. Consider reaching out to the insurance provider directly after a couple of weeks to inquire about the status of your claim. If your appeal is denied, understand your rights and the next steps available to you, which might include further appeals or seeking external reviews.
Helpful links and resources
Navigating the appeals process can be daunting, but various resources are available to guide you. Consider exploring additional guidance provided by healthcare advocates and legal experts who specialize in insurance appeals. These resources can offer vital support and knowledge to bolster your case.
Make use of important contacts for assistance, like your healthcare provider, social workers, and patient advocates, who can offer insights and possibly help in fostering a successful appeal.
Staying updated and informed
To remain stay informed regarding changes to the appeals process and insurance regulations, consider subscribing to relevant newsletters and updates. Many organizations dedicated to patient advocacy offer useful insights into policy changes and practical advice.
Engaging with online communities and support groups provides valuable networking opportunities and experiences. Sharing your success stories can those grappling with similar challenges a tremendous sense of hope and encouragement.
Interactive tools and frequently asked questions
Utilizing interactive tools such as checklists and worksheets can dramatically enhance your preparedness for submitting a coverage determination appeal. pdfFiller offers templates that can guide you from start to finish in the process.
Addressing frequently asked questions surrounding the coverage determination appeal form can clarify common concerns and procedural outlines. Engaging with platforms that foster user feedback will further enhance the shared knowledge base.






For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
How can I manage my coverage determination appeal directly from Gmail?
How do I complete coverage determination appeal on an iOS device?
Can I edit coverage determination appeal on an Android device?
What is coverage determination appeal?
Who is required to file coverage determination appeal?
How to fill out coverage determination appeal?
What is the purpose of coverage determination appeal?
What information must be reported on coverage determination appeal?
pdfFiller is an end-to-end solution for managing, creating, and editing documents and forms in the cloud. Save time and hassle by preparing your tax forms online.