Get the free medicare-prescription-drug-redetermination-appeals- ...
Get, Create, Make and Sign medicare-prescription-drug-redetermination-appeals



How to edit medicare-prescription-drug-redetermination-appeals online
Uncompromising security for your PDF editing and eSignature needs
How to fill out medicare-prescription-drug-redetermination-appeals

How to fill out medicare-prescription-drug-redetermination-appeals
Who needs medicare-prescription-drug-redetermination-appeals?
Medicare Prescription Drug Redetermination Appeals Form - How-to Guide
Understanding the Medicare Prescription Drug Redetermination Appeals Form
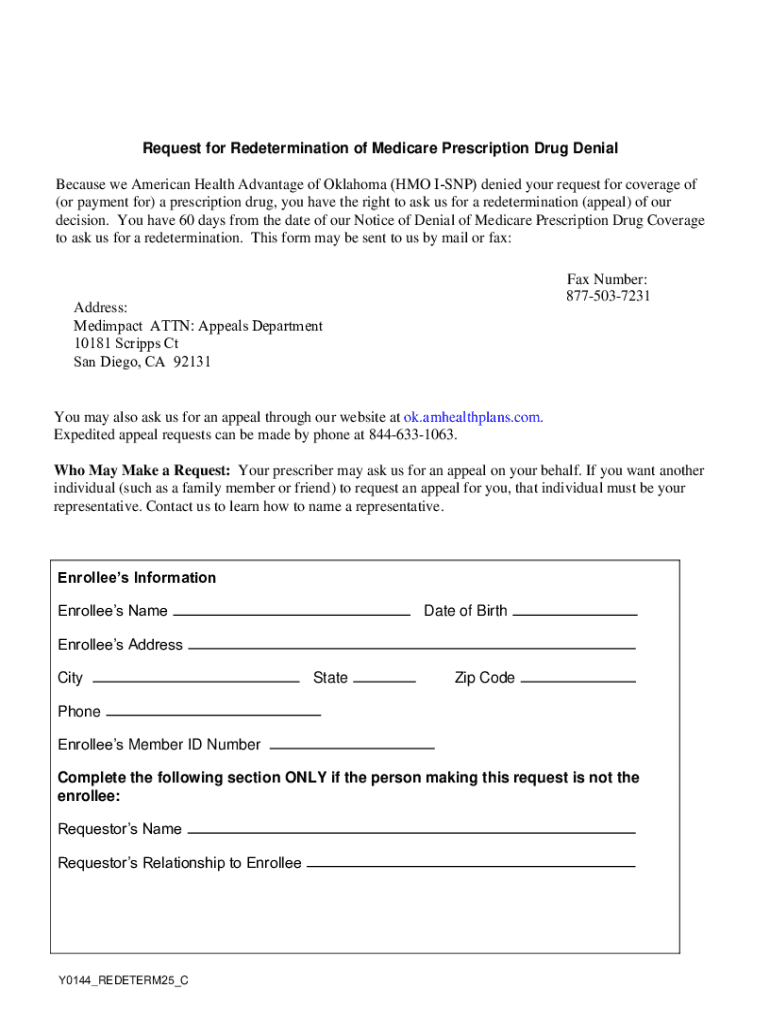
The Medicare Prescription Drug Redetermination Appeals Form serves as a pivotal tool for individuals seeking to challenge decisions made by their Medicare drug plan regarding coverage. When a Medicare beneficiary is denied coverage for a particular prescription medication, this form allows them to formally request a review of the decision. This process is an important right for patients, ensuring they have access to necessary medications.
The significance of this form in the appeals process cannot be understated. It acts as the first step in advocating for a patient's rights and ensuring that they receive the drugs needed for their health conditions. Understanding this form is crucial for anyone looking to navigate the often-complex Medicare system effectively.
Key terminology
Navigating the Medicare system and appeals process can seem daunting, especially given the specific terminology involved. Key terms include 'redetermination', which refers to the process of reviewing the initial decision made by a plan regarding drug coverage. This term signifies a chance for the beneficiary to present their case against the denial of medication.
Others terms include 'appeal', which is a formal request to reconsider a denied request, and 'supplier', which refers to the pharmacy or healthcare provider dispensing the medication. Familiarity with these terms can enhance an individual's understanding of their rights and the processes involved.
When to use the Medicare Prescription Drug Redetermination Appeals Form
Knowing when to utilize the Medicare Prescription Drug Redetermination Appeals Form is crucial for every Medicare beneficiary. Eligibility to file an appeal generally requires the individual to be enrolled in a Medicare plan when the denial of medication occurs. This form should be filed when a member believes that their insurance plan is unjustly refusing coverage for a prescribed drug.
Each of these scenarios highlights the necessity of submitting an appeal. Recognizing such instances allows beneficiaries to maintain control over their healthcare decisions and ensure they have access to necessary treatments.
How to complete the Medicare Prescription Drug Redetermination Appeals Form
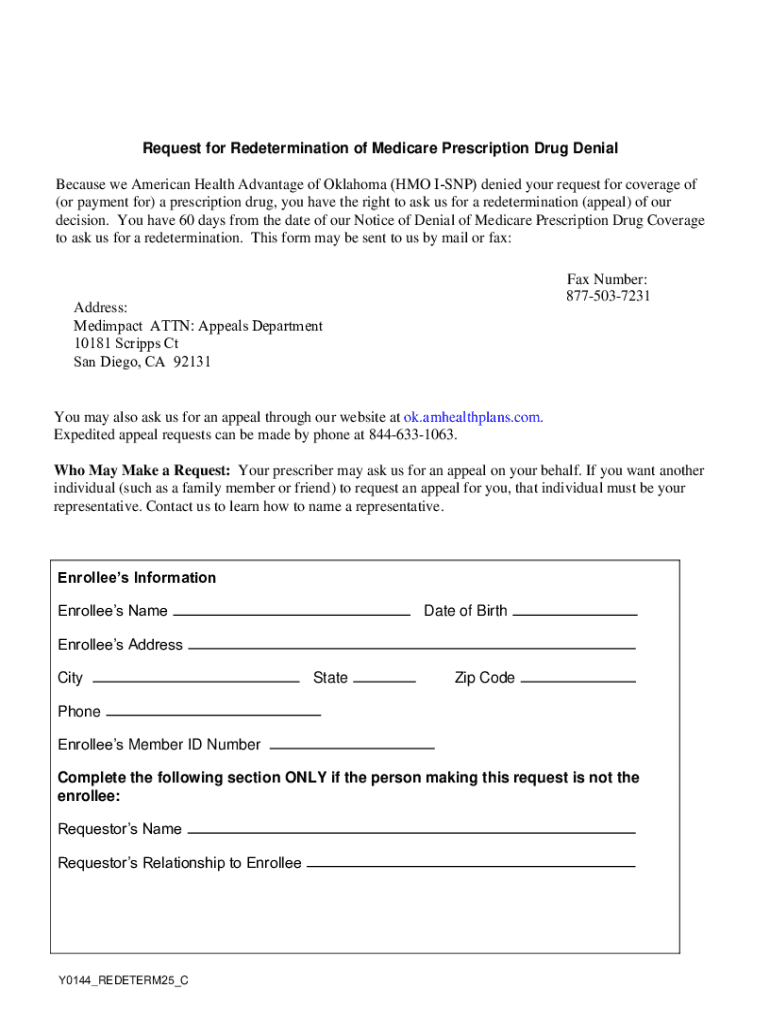
Completing the Medicare Prescription Drug Redetermination Appeals Form involves carefully following structured instructions to ensure accurate submission. The form is typically broken down into four main sections. In Section 1, personal information is collected, which includes the beneficiary's name, Medicare number, and contact details, ensuring the appeal can be traced back to the individual.
Section 2 requires detailed drug information, including the name of the medication, the prescribed dosage, and the reason for its necessity. Moving on to Section 3, beneficiaries must provide a reason for the appeal that clearly outlines the justification for reconsideration. Finally, Section 4 is crucial, as it requests any supporting documentation, such as prescriptions or letters from healthcare providers, which substantiate the request.
Proper completion of this form can significantly influence the outcome of the appeal, making attention to detail paramount.
Tips for accuracy
Ensuring the accuracy of the Medicare Prescription Drug Redetermination Appeals Form is essential for success. It’s crucial to double-check all entries for completeness and clarity. Verify that personal details are correct, and descriptions of medications and reasons for appeal are specified clearly. Miscommunications or unclear requests can lead to unnecessary delays or denials.
One practical approach is to draft your responses on a separate document before filling out the form. This allows for thorough review and adjustments. Additionally, seek feedback from a healthcare provider or an advocate familiar with the Medicare process, as they might catch errors or suggest enhancements to strengthen the appeal.
Documenting your appeal
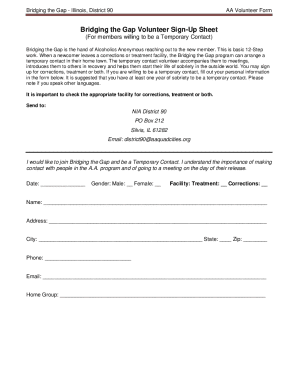
Documentation plays an integral role in the appeal process. When submitting the Medicare Prescription Drug Redetermination Appeals Form, accompanying documentation can dramatically bolster your case. It is important to include a comprehensive list of all relevant documents such as prescriptions, medical records, and letters from your healthcare provider.
The collection of these documents is not only crucial for a robust appeal but helps illustrate the context of the situation. Collaborating with healthcare providers is often necessary to procure these documents, and their insights can be invaluable.
Submitting your Medicare Prescription Drug Redetermination Appeals Form
Once the Medicare Prescription Drug Redetermination Appeals Form is accurately filled and supported by necessary documentation, submission can take several forms. Online submissions are available via the Medicare portal, allowing for immediate processing in many cases. Alternatively, beneficiaries can mail or fax the appeal directly to their insurance provider.
Regardless of the method chosen, beneficiaries should always secure proof of submitting their appeal. This documentation will be crucial in tracking the progress of their appeal and ensuring accountability from the provider.
Timeline of the appeals process
Understanding the timeline for the Medicare appeals process is vital for managing expectations. Typically, after submitting the Medicare Prescription Drug Redetermination Appeals Form, beneficiaries should expect to receive a decision within a few weeks. The exact timeframe can vary based on the complexity of the case and the efficiency of the provider's administrative team.
Keeping track of these timelines will help beneficiaries follow up accordingly. Utilizing tools such as those provided by pdfFiller can aid in managing documents and reminders for follow-ups, thereby streamlining the entire appeal process.
Troubleshooting common issues
Despite thorough preparation, some appeals may still get denied. In such cases, it's essential to understand the options available for further action. If an appeal is denied, beneficiaries should carefully review the reasoning provided and determine whether it is possible to submit a secondary appeal or provide additional information to address the concerns outlined by the insurance provider.
On the other hand, if the appeal process is delayed beyond the expected timeframe, beneficiaries should not hesitate to reach out to their provider or Medicare for assistance. They have avenues for tracking and ensuring the appeal is processed appropriately.
Helpful links and resources
For beneficiaries navigating the Medicare Prescription Drug Redetermination Appeals Form, utilizing available resources is advisable. The official Medicare website provides official documents and guidance on the appeals process. These resources serve as comprehensive references throughout the appeal journey.
Engaging with other beneficiaries can provide real-world strategies and encouragement as individuals navigate their own unique situations.
Using pdfFiller for your Medicare appeals journey
pdfFiller can significantly enhance the experience of submitting the Medicare Prescription Drug Redetermination Appeals Form. The platform provides users with an easy-to-navigate interface for creating, editing, and managing all necessary appeal documentation efficiently. This user-friendly approach ensures that individuals can complete forms accurately and in a manner that complies with requirements.
Additionally, pdfFiller includes collaborative tools where family members or healthcare advocates can assist in reviewing and submitting forms, ensuring a thorough approach to the process.
Subscription for ongoing updates and information
Staying informed about changes to Medicare policies is crucial for beneficiaries. Subscribing to updates through Medicare newsletters or using platforms like pdfFiller to receive email notifications ensures you are consistently aware of developments that might influence your appeals process.
Moreover, utilizing additional tools and templates offered by pdfFiller can streamline the management of various healthcare documents, promoting overall preparedness in healthcare matters.






For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
How can I manage my medicare-prescription-drug-redetermination-appeals directly from Gmail?
How do I complete medicare-prescription-drug-redetermination-appeals online?
How do I fill out the medicare-prescription-drug-redetermination-appeals form on my smartphone?
What is medicare-prescription-drug-redetermination-appeals?
Who is required to file medicare-prescription-drug-redetermination-appeals?
How to fill out medicare-prescription-drug-redetermination-appeals?
What is the purpose of medicare-prescription-drug-redetermination-appeals?
What information must be reported on medicare-prescription-drug-redetermination-appeals?
pdfFiller is an end-to-end solution for managing, creating, and editing documents and forms in the cloud. Save time and hassle by preparing your tax forms online.