Get the free Claim Appeals, Reconsiderations & Disputes
Get, Create, Make and Sign claim appeals reconsiderations amp



Editing claim appeals reconsiderations amp online
Uncompromising security for your PDF editing and eSignature needs
How to fill out claim appeals reconsiderations amp

How to fill out claim appeals reconsiderations amp
Who needs claim appeals reconsiderations amp?
Claim Appeals Reconsiderations AMP Form: Your Complete Guide
Understanding claim appeals and reconsiderations
Claim appeals provide an essential avenue for individuals and teams to contest denied claims. When an insurance company or government program refuses to authorize a claim, the claimant can file an appeal to dispute that decision. The purpose of reconsiderations is to review the initial determination with potentially new evidence or clarification of existing information, often leading to a different outcome.
Common scenarios for filing appeals include denied health insurance claims based on coverage exclusions, rejected workers' compensation claims, or denials of disability benefits. It's essential to request a reconsideration promptly following the denial to preserve your rights to an appeal, as most entities have strict timelines within which these requests must be submitted.
The importance of the AMP form in the claims process
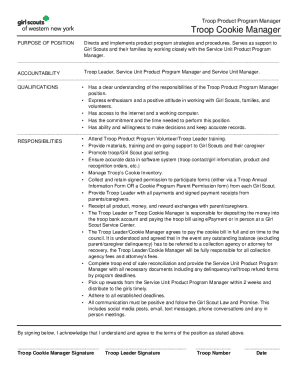
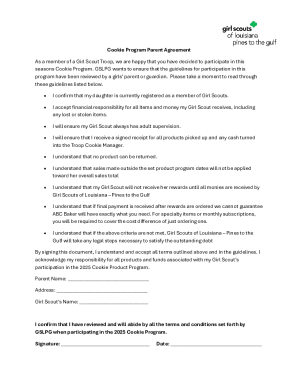
The AMP form is a key component of the claims process, offering a structured way to submit your appeal and provide necessary details. This form aids in clearly presenting your justification for reconsideration and ensures the appropriate information reaches the claims reviewer efficiently.
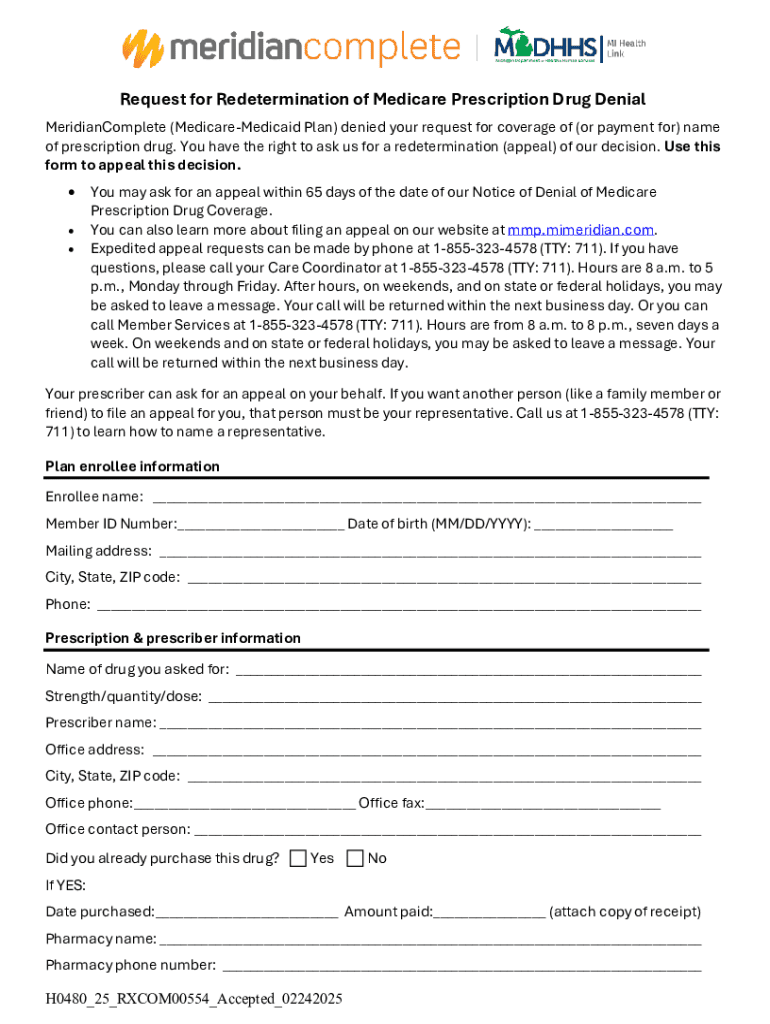
Key components of the AMP form typically include personal information, claim specifics, reasons for reconsideration, and supporting documentation. Unlike other forms, the AMP form is designed to encapsulate all necessary details in one document, improving clarity for both the claimant and the reviewing parties.
Step-by-step guide to filling out the AMP form
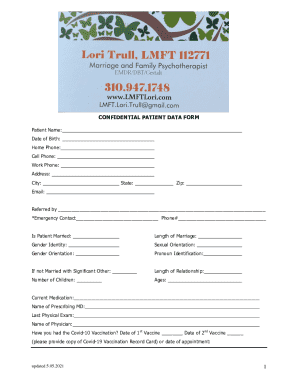
Filling out the AMP form requires attention to detail and organization. In Section 1, begin with your claimant information. You'll need to enter required personal identifiers like your name, address, and contact details. It's crucial to ensure all entries are accurate to avoid delays.
In Section 2, describe your claim thoroughly, incorporating relevant dates and specific details that explain the claim’s context. The more precise you can be, the better your chances of a successful appeal. Moving to Section 3, articulate your reasons for reconsideration clearly, using structured arguments that focus on why the original decision should be challenged.
In Section 4, attach the necessary supporting documentation. This can include treatment histories, expense receipts, or additional reports that substantiate your case. Ensure your documents are organized and easy to reference.
Editing and formatting your AMP form
Using tools like pdfFiller can streamline the editing process of your AMP form. Take advantage of the platform's features to make necessary adjustments and ensure your content is formatted correctly. This means utilizing ample white space, logical breaks between sections, and consistency in font and style.
Best practices for formatting include checking for grammatical errors, spelling mistakes, and ensuring that the information flows logically. Clarity and professionalism in your presentation can impact how your appeal is received, presenting you as detail-oriented and serious about your claim.
Adding signatures and verifying your AMP form
Once you have filled out the AMP form, the next step is to add your signature. You can use pdfFiller's eSignature tools, which allow you to create and insert a legally binding signature into your document with ease. Ensure that you also verify any requirements for witness signatures if applicable, as many claims processes necessitate additional verification.
It's crucial to confirm that your signatures meet compliance standards. This generally includes ensuring the signatures are dated and positioned correctly on the form, which can vary depending on the guidelines provided by the claims reviewer.
Managing your claims process post-submission
Once you've submitted your AMP form, tracking the status of your appeal is essential. Many insurance companies and government agencies provide online portals where you can view the progress of your claim. Knowing where your request stands can help you manage your expectations and prepare for any next steps.
What to expect after submission can vary, but generally, you should anticipate a confirmation of receipt followed by a timeline for when a decision will be made. Following up effectively can involve reaching out via phone or email, particularly if you're approaching deadlines or have not received communication within the expected timeframe.
Common mistakes to avoid when filing claims appeals
The process of filing a claims appeal can be hindered by common mistakes, especially in the AMP form. Incomplete forms, missing signatures, or incorrect personal information can lead to delays or denials. It's vital to double-check your form before submitting to catch any potential errors.
Ensuring your submission is complete is critical. Each section of the AMP form should be thoroughly filled out, and all required documents included. The impact of missing information can lead to a significant setback in your appeal process, so be meticulous in your preparation.
Troubleshooting common issues with the AMP form
If your appeal encounters rejection from insurance providers, it's essential to understand the reasons cited for denial. Reviewing the rejection notice can provide insight into what needs to be addressed or clarified in your appeal. If you don't receive a response within a reasonable timeframe, consider contacting the claims office directly to request an update.
In some cases, re-submitting your claim or reconsideration request may be necessary. When doing so, ensure to address any previous concerns raised and clarify any new or additional information that could support your case. Consistent follow-up on resubmissions can also benefit your claim process.
Utilizing pdfFiller for claim appeals
pdfFiller offers a suite of features tailored for managing claims appeals effectively. The ability to edit PDFs, eSign documents securely, collaborate with team members on appeals, and store forms in one accessible location significantly enhances the claims process. These tools make it easier to stay organized and efficient.
Benefits of using a cloud-based solution like pdfFiller include access to your documents from anywhere, the ability to collaborate in real-time, and enhanced security features to protect sensitive information. Such a platform empowers both individuals and teams to handle their claims processes with confidence and flexibility.
Inspiring success stories
Many individuals have used the AMP form successfully to overturn claim denials. For instance, consider the story of a family who appealed a health insurance denial due to a pre-existing condition. By leveraging the AMP form and presenting robust, well-documented evidence, they not only succeeded in overturning the initial denial but also influenced policy adjustments within their provider’s coverage guidelines.
Lessons learned from these experiences highlight the importance of thorough documentation, the correct usage of forms, and the value of timely submissions. By understanding the processes and employing the right tools like pdfFiller, claimants can navigate these challenging situations more effectively.






For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
Where do I find claim appeals reconsiderations amp?
How do I edit claim appeals reconsiderations amp online?
How do I complete claim appeals reconsiderations amp on an Android device?
What is claim appeals reconsiderations amp?
Who is required to file claim appeals reconsiderations amp?
How to fill out claim appeals reconsiderations amp?
What is the purpose of claim appeals reconsiderations amp?
What information must be reported on claim appeals reconsiderations amp?
pdfFiller is an end-to-end solution for managing, creating, and editing documents and forms in the cloud. Save time and hassle by preparing your tax forms online.