Get the free Home Care Prior Authorization Form Guide
Get, Create, Make and Sign home care prior authorization
Editing home care prior authorization online
Uncompromising security for your PDF editing and eSignature needs
How to fill out home care prior authorization
How to fill out home care prior authorization
Who needs home care prior authorization?
Home Care Prior Authorization Form: How-to Guide
Overview of home care prior authorization
Prior authorization serves as a crucial checkpoint in the home care process. It is necessary for ensuring that patients receive the level of care that is consistent with their medical needs while aligning with the coverage policies of their health insurance providers.
Many people fail to understand the significance of obtaining prior authorization before engaging home care services. This process is vital not just for approval but also for ensuring that families and caregivers are covered for the expenses incurred during home care.
Understanding the home care prior authorization process
Prior authorization involves a formal approval process that health insurance companies require before they agree to pay for certain medical services or procedures. In the context of home care, this may include skilled nursing services, physical therapy, or home health aide visits.
It's essential to differentiate prior authorization from pre-certification. While both processes involve obtaining approval from an insurer, pre-certification is typically required for planned hospital admissions or specialized procedures, while prior authorization is more frequently applied to ongoing and outpatient services.
Compliance with prior authorization requirements is critical not only to avoid potential denials of services but also to ensure continuity of care during challenging times for patients and families.
Key players in the prior authorization process
Several individuals and organizations play significant roles in the prior authorization ecosystem. Healthcare providers, including doctors and specialists, initiate the authorization process by documenting medical necessity.
Insurance companies assess these requests based on their policies and guidelines, which can differ tremendously between providers. Patients and their families are crucial as they navigate the complexities of approvals, while home care agencies facilitate the delivery of authorized services.
When is prior authorization required for home care services?
Certain home care services frequently require prior authorization. These often include skilled nursing visits, physical therapy treatments, and durable medical equipment rentals. However, the specific services that require prior authorization can vary based on the insurer and the particular plan.
It's also vital to consider exceptions to prior authorization requirements. Some acute care situations, along with emergency services, may not necessitate prior approvals due to the immediate need for response.
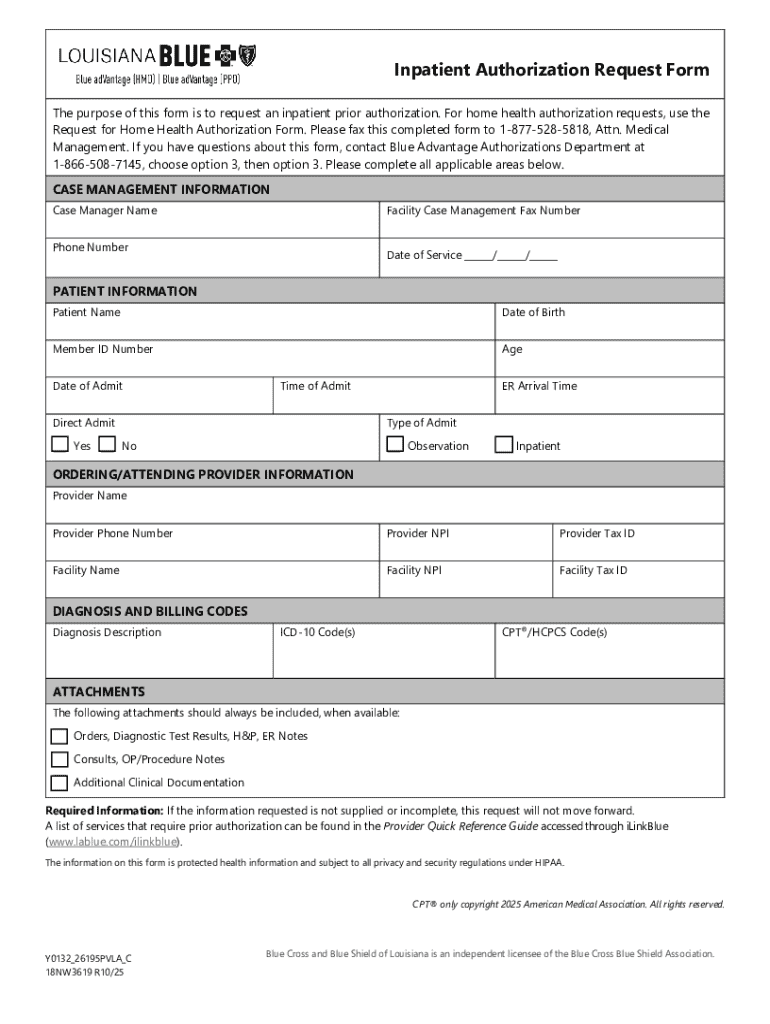
Essential elements of the home care prior authorization form
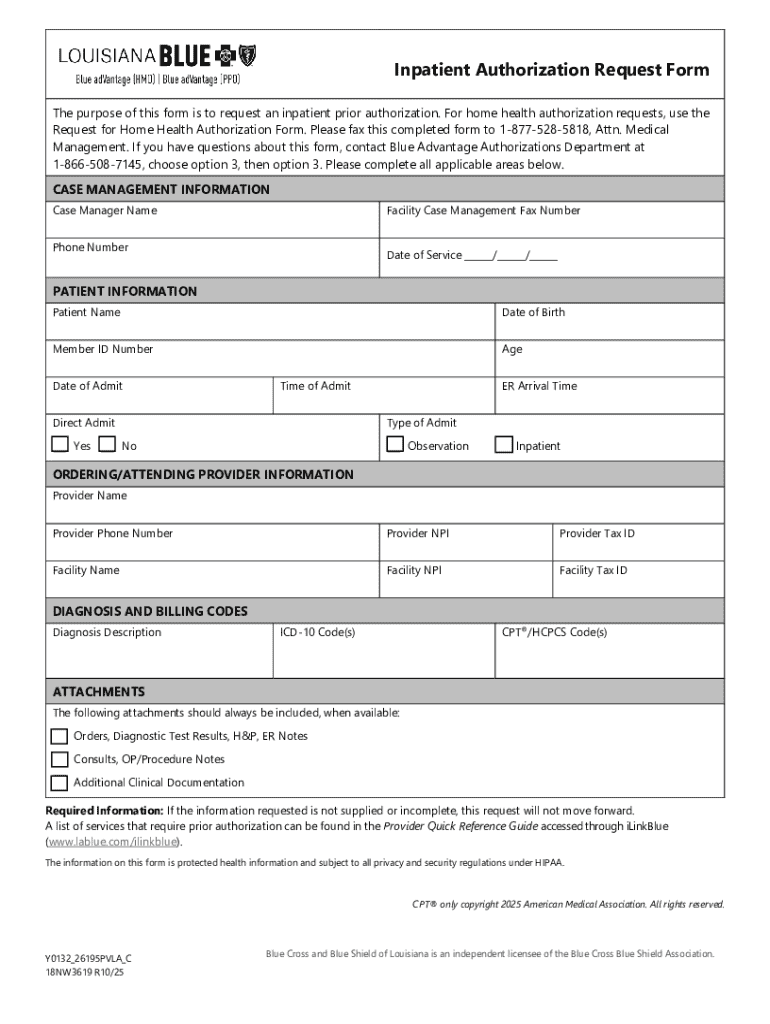
Completing a home care prior authorization form accurately is vital to facilitate quicker processing. The form typically includes sections where personal information about the patient must be captured, alongside detailed healthcare provider information. Each requested service should be enumerated explicitly within the form.
Additionally, supporting medical documentation, such as physician notes or diagnostic tests, should accompany the form. This information demonstrates the medical necessity for services requested and aids in expediting the review process.
Step-by-step guide to completing the home care prior authorization form
To efficiently complete a home care prior authorization form, it's critical to gather necessary information beforehand. Start by collecting personal details about the patient, such as the complete name, date of birth, and any relevant diagnosis codes. Insurance information, including policy numbers and group identifiers, should also be gathered from the patient’s insurance card.
Next, you'll want to detail the services being requested. Be as specific as possible—include the frequency, duration, and any other relevant details that might support the request.
When filling out the form, ensure accuracy in common fields, reviewing to avoid typos or omissions. Submit the completed form electronically if possible or mail it using a designated process. Maintain records of all submissions to ensure follow-up is manageable.
Common challenges in the prior authorization process
Prior authorization is not without its challenges. Delays in approval can occur, leaving patients uncertain about when they will receive needed care. Incomplete documentation often leads to rejections; therefore, it’s crucial that all required information is accurately submitted to avoid unnecessary holdups.
Furthermore, the denial of requests can be disheartening for patients and families. Navigating the appeals process is often complex and requires a thorough understanding of the justification for services based on medical necessity.
Important considerations post submission
After submitting a home care prior authorization form, ongoing monitoring of its approval status is essential. This can often be achieved through direct contact with the insurance provider, which might involve a follow-up call or check-in via their web portals.
Understanding your rights regarding prior authorization is also important. Patients have the right to accessible explanations of denials and the potential options available to them. Preparing for possible denials by having additional documentation at hand can facilitate faster resolutions.
Leveraging technology for home care prior authorization
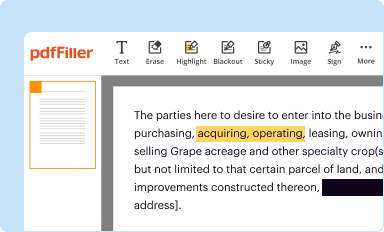
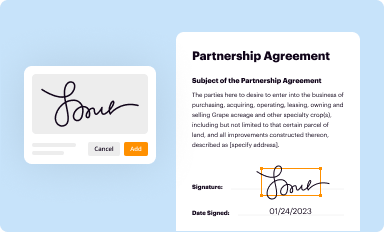
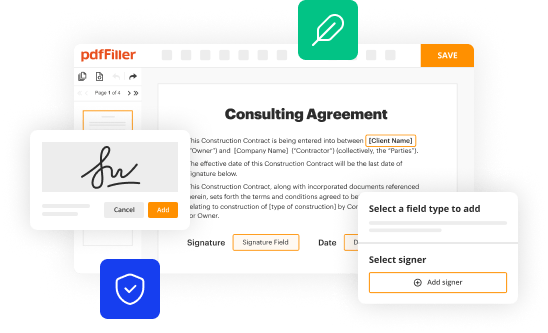
Utilizing technology can significantly streamline the home care prior authorization process. Online platforms like pdfFiller enhance the experience by offering seamless document editing, allowing users to fill, sign, and manage authorization forms easily.
Furthermore, features like integrated e-signing capabilities and collaborative tools can transform how healthcare teams communicate while managing these essential documents. Real-time collaboration assures all stakeholders are in sync and can expedite the authorization process.
FAQs about home care prior authorization
Home care prior authorization can raise various questions. For instance, what if a request is denied? Understanding the specific reasons for denials often allows for quick resubmissions with additional or clarifying documentation.
Additionally, many ask how long the approval process typically takes. While it can vary by insurance carrier, being proactive in following up can often yield more timely insight into the approval timeline.
Case studies: successful prior authorizations
Analyzing successful prior authorization cases provides insights into what works best. In one example, a patient requiring ongoing physical therapy received quick approval due to a thorough initial submission that included not only standard forms but also comprehensive medical notes.
Conversely, lessons learned from denied requests emphasize the need for meticulous attention to detail. A request that was initially denied due to missing documentation from the primary care provider was later approved when that information was included.
Final tips for a smooth prior authorization experience
For a successful home care prior authorization experience, starting the process early is critical. Late submissions can lead to gaps in care. Keeping organized, with all necessary documentation in a single location, helps speed up the process.
Additionally, maintaining open communication with insurers allows families to clarify doubts promptly. Utilizing comprehensive document solutions such as pdfFiller can significantly enhance the overall document management experience, ensuring that no detail gets overlooked.






For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
How can I edit home care prior authorization from Google Drive?
How do I edit home care prior authorization online?
How can I fill out home care prior authorization on an iOS device?
What is home care prior authorization?
Who is required to file home care prior authorization?
How to fill out home care prior authorization?
What is the purpose of home care prior authorization?
What information must be reported on home care prior authorization?
pdfFiller is an end-to-end solution for managing, creating, and editing documents and forms in the cloud. Save time and hassle by preparing your tax forms online.