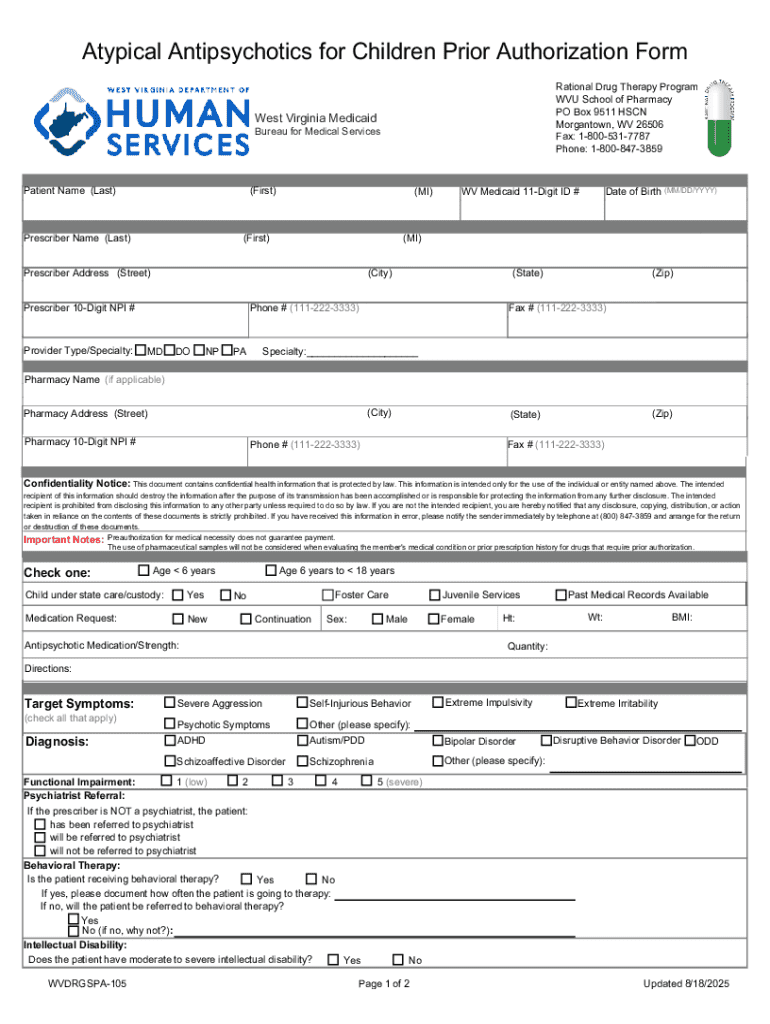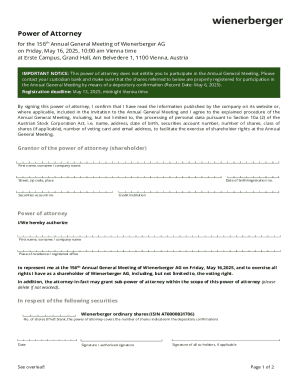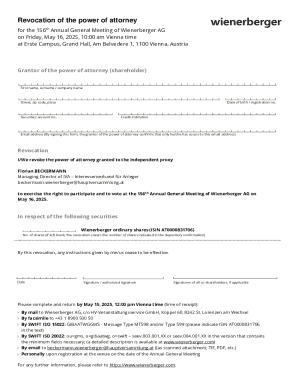
Get the free Prior Authorization Forms - WV Medicaid Application
Get, Create, Make and Sign prior authorization forms
How to edit prior authorization forms online
Uncompromising security for your PDF editing and eSignature needs
How to fill out prior authorization forms
How to fill out prior authorization forms
Who needs prior authorization forms?
Prior Authorization Forms Form: A Comprehensive How-to Guide
Understanding prior authorization forms
Prior authorization forms are critical documents in the healthcare system that ensure that medical services and procedures are medically necessary and appropriately covered by insurance plans before they are provided. These forms act as a gatekeeping mechanism, often determining whether a patient will receive needed treatments, medications, or diagnostics based on the recommendations of their healthcare provider.
In the fast-evolving landscape of healthcare, the significance of prior authorization forms cannot be overstated. They help in regulating healthcare expenditures, ensuring that resources are allocated judiciously while aiming to curtail unnecessary treatments. This process not only benefits insurance companies by managing costs but also promotes accountability in healthcare delivery, fostering a more judicious approach to patient care.
Insurance providers play a pivotal role in the prior authorization process. They establish specific criteria for the types of services that require authorization, thereby ensuring that medical necessity and appropriateness are prioritized. Understanding these criteria is crucial for healthcare teams as they navigate the complexities of patient care and billing processes.
When is prior authorization necessary?
Certain medical procedures, medications, and tests often necessitate prior authorization due to their high costs or because they involve specialized care. Common scenarios where prior authorization is typically required include surgeries, advanced imaging (like MRIs and CT scans), certain specialty medications, and high-cost therapeutic treatments.
Understanding when prior authorization is necessary is vital for both healthcare providers and patients. Delays in obtaining these authorizations can significantly impact patient care. If a requested procedure is delayed, patients may experience a worsening of their condition or an increase in treatment costs. Additionally, these delays can lead to frustration among patients and healthcare providers alike.
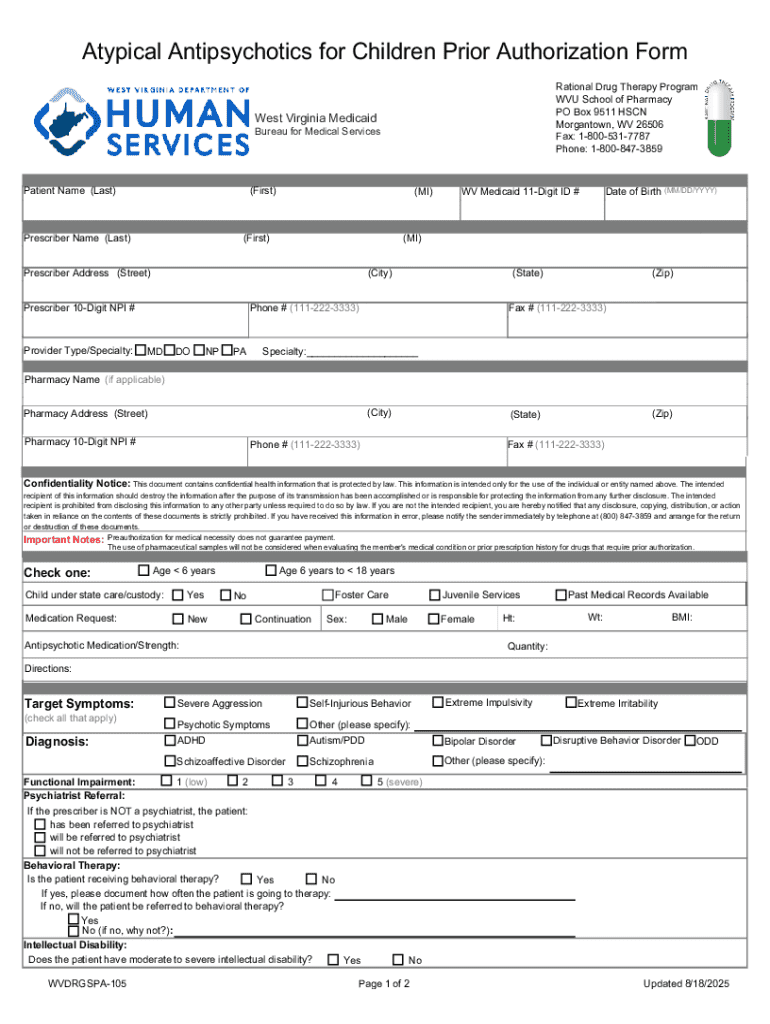
The process of requesting prior authorization
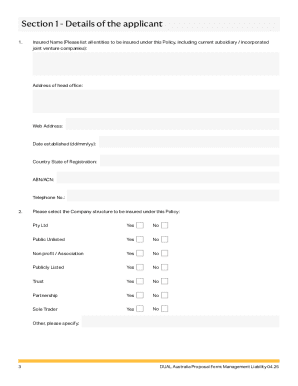
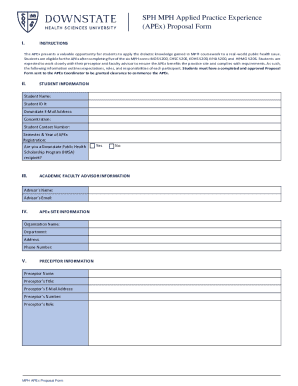
Requesting prior authorization involves several critical steps to ensure that the process runs smoothly and efficiently. The first step is gathering all necessary information, which includes patient details, insurance information, medical history, and specific treatment details. This information not only supports the request but also aids in justifying the medical necessity of the treatment being sought.
Once the necessary information is collected, the next step is completing the prior authorization form. Each section of the form must be filled out accurately, and it’s beneficial to use interactive guides that break down the form's components. This may include sections for patient identification, details about the requested service, clinical rationale, and supporting documents.
Finally, following up on the status of the submission is essential. This can involve calling the insurance company or checking their online portal for updates. These follow-ups ensure that requests do not languish in processing and that any delays can be addressed promptly.
Tips for a successful prior authorization request
Navigating the prior authorization process successfully often hinges on avoiding common pitfalls that can lead to denials. First, it’s critical to ensure that all sections of the prior authorization form are filled out completely and accurately. Missing information or typos can easily result in a denied request and cause delays for the patient.
Supporting documentation can make or break a prior authorization request. Ensuring that you include comprehensive medical records, previous treatment outcomes, and any relevant clinical studies can strengthen your case for medical necessity. Additionally, familiarizing yourself with the specific guidelines for different insurers can enhance your submission. Each provider may have unique requirements regarding documentation or justification needed for similar procedures.
Managing denials and appeals
Denials can be frustrating, but understanding common reasons for these determinations can help prepare for an appeal. Typical reasons for denial include lack of medical necessity, incomplete information, or non-compliance with insurance guidelines. Identifying these issues upfront can enhance the chances of a successful appeal.
To effectively appeal a denial, it’s important to follow these steps meticulously. First, gather all necessary documentation that may include revised or additional medical records, statements from the healthcare provider, and any new supporting documents or clinical evidence that can bolster your case. Each insurance company may have specific timelines and procedures for submitting appeals, so it's crucial to follow their guidelines closely.
Engaging with both healthcare providers and payers is essential during this process. Effective communication can help clarify misunderstandings and facilitate a smoother appeals process, ultimately improving outcomes for the patient involved.
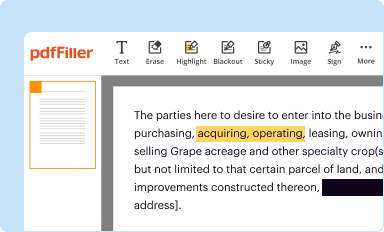
Digital tools for managing prior authorizations
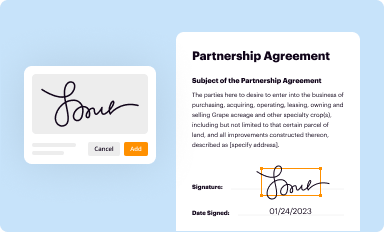
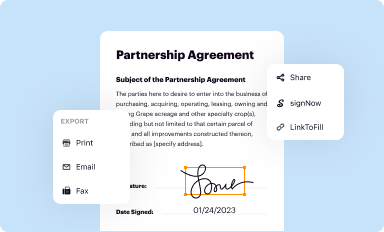
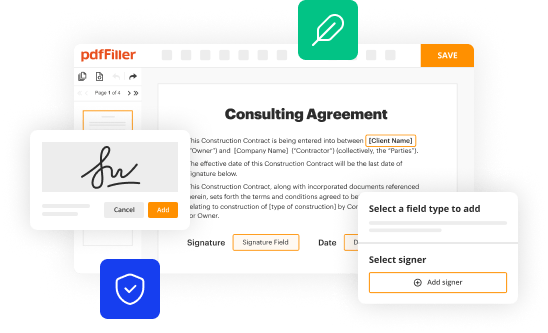
In the era of digital health solutions, pdfFiller stands out as a versatile tool for managing prior authorization forms efficiently. Its user-friendly platform allows healthcare teams to edit, sign, and store documents seamlessly. With pdfFiller, users can easily edit prior authorization forms to fit specific needs, ensuring precision and compliance.
One of the standout features of pdfFiller is its electronic signing capability, which allows for faster processing times. This feature not only expedites the prior authorization process but also enhances convenience for busy healthcare professionals who may need to manage documents on the go. With access to forms from anywhere, healthcare teams can quickly collaborate with one another, sharing vital information and updates as needed.
Frequently asked questions (FAQs)
The prior authorization process often raises many questions from patients and providers alike. Understanding what happens if a prior authorization is not approved is essential, as it may mean seeking alternative treatments or appealing the decision. The timeline for the authorization process varies, but knowing that it typically takes anywhere from a few hours to several days can help manage expectations.
Another common inquiry is about the use of prior authorization forms for multiple requests. Generally, each request will require its own form unless specifically stated otherwise by the insurance provider. Additionally, if an insurance company requests further information, having a clear protocol for gathering and submitting that information can ease communication and expedite the approval process.
Future of prior authorization processes
As healthcare continues to evolve, so too does the process of prior authorizations. Trends indicate a growing push for simplification and automation within the field. Many insurers are looking into streamlining the prior authorization process by increasing automation, which, in turn, aims to reduce administrative burdens on healthcare professionals.
Technological advancements are also driving changes. Digital tools that integrate real-time data sharing and automated decision-making are emerging, helping to decrease the turnaround time for authorization requests significantly. This push for simplification reflects a broader recognition of the need for a more patient-centric approach that alleviates the burdens traditionally associated with prior authorization processes.






For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
How can I edit prior authorization forms from Google Drive?
How do I fill out prior authorization forms using my mobile device?
How do I fill out prior authorization forms on an Android device?
What is prior authorization forms?
Who is required to file prior authorization forms?
How to fill out prior authorization forms?
What is the purpose of prior authorization forms?
What information must be reported on prior authorization forms?
pdfFiller is an end-to-end solution for managing, creating, and editing documents and forms in the cloud. Save time and hassle by preparing your tax forms online.