Get the free COBRA Open Enrollment Form: Health Election for Medical ...
Get, Create, Make and Sign cobra open enrollment form
Editing cobra open enrollment form online
Uncompromising security for your PDF editing and eSignature needs
How to fill out cobra open enrollment form
How to fill out cobra open enrollment form
Who needs cobra open enrollment form?
Navigating the COBRA Open Enrollment Form: A Comprehensive Guide
Understanding COBRA open enrollment
COBRA, or the Consolidated Omnibus Budget Reconciliation Act, is a federal law that enables individuals to maintain their health insurance coverage when they experience certain qualifying events. This ensures continuity in health coverage, allowing individuals to avoid gaps in their insurance after employment changes, such as job loss or reduced work hours.
The significance of COBRA cannot be overstated. It acts as a safety net for individuals and families who might find themselves suddenly facing healthcare expenses due to unforeseen changes in their employment status. Without COBRA, these individuals would need to navigate the often complex landscape of finding new health insurance, which can lead to missed medical care and financial strain.
Eligibility for COBRA open enrollment
Determining eligibility for COBRA is crucial to making the most of this benefit. Generally, the law applies to employees of companies with 20 or more employees who have been covered by the group's health plan for at least 60 days prior to the qualifying event.
There are specific guidelines about who qualifies under COBRA. Primarily, full-time employees are eligible, alongside certain part-time employees based on hours worked. Dependents are also eligible, provided they were covered under the same group health plan prior to the qualifying event. Understanding these criteria is essential as it may affect how individuals complete the COBRA open enrollment form.
Navigating the open enrollment process
The enrollment timeline for COBRA is critical to ensure you don’t miss your opportunity for continued health coverage. Generally, individuals have 60 days from the date of the qualifying event or from when they receive their COBRA election notice to enroll. Knowing these dates helps individuals plan effectively.
The first step to filling out the COBRA enrollment form is to gather necessary documents. This includes proof of your previous health plan, which may involve pay stubs or previous insurance cards. Once you have these documents, you can begin completing the form.
The form will typically require personal information, coverage selection based on whether you want individual or family plans, and an acknowledgment of your rights and responsibilities regarding the coverage. The submission methods vary; you can send your completed form via online interfaces, mail, or fax, depending on your previous plan’s management.
Managing your COBRA coverage
After enrolling in COBRA, understanding your options is paramount. First, you need to familiarize yourself with your coverage options, including details about medical services, prescription drugs, and any deductibles or coinsurance requirements specific to your plan.
Being aware of premium payment responsibilities is essential. COBRA premiums can be higher than what you were paying as an employee since they may include the full cost of coverage plus a 2% administrative fee. Tools available at pdfFiller can help you manage your COBRA documents and track payments effectively.
Special considerations during open enrollment
One of the critical aspects during the COBRA enrollment period is considering how it affects your dependents. Individuals have the option to add or remove dependents from their policy during this time, which is essential for ensuring that all family members have the necessary coverage.
Avoiding gaps in coverage is also a priority. It's possible to have overlapping policies if you secure new insurance while on COBRA, but understanding the rules about switching without facing penalties is paramount. Special enrollment periods can occur with certain life events, which might allow additional flexibility in enrolling in different insurance plans.
Frequently asked questions (FAQs)
Many individuals have questions about the implications of COBRA, especially regarding missed deadlines. If you miss the enrollment period, you may lose your chance to enroll in COBRA. However, there might be options available for you to obtain new health insurance, depending on your circumstances.
COBRA coverage can generally last for up to 18 months, depending on the qualifying event. It's also possible to switch to another health plan after your COBRA coverage ends, but it's advisable to consider your options before your COBRA coverage expires to prevent lapses in insurance.
Leveraging pdfFiller for your COBRA needs
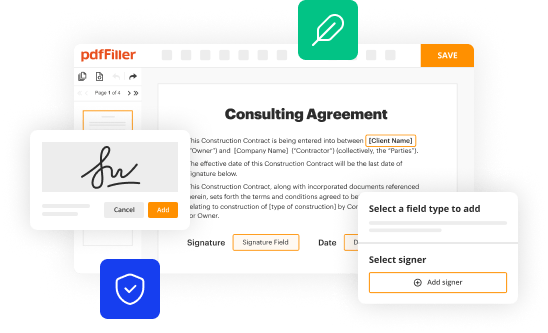
pdfFiller offers a streamlined approach for managing COBRA forms and related documents. The platform allows users to edit forms easily and apply electronic signatures, making the entire process much more efficient. Collaboration tools can assist teams that are managing multiple COBRA enrollments, ensuring everyone stays aligned.
Accessing support through pdfFiller is straightforward as the platform provides various templates and resources related to COBRA. Whether you need guidance for filling out forms or help with document-related inquiries, customer support is readily available to assist users in navigating their COBRA options and responsibilities effectively.
Conclusion: Empowering your journey with COBRA
Understanding the COBRA open enrollment form is essential for those facing transitions in their employment. By being aware of eligibility, navigating the enrollment process, and managing the coverage effectively, individuals can ensure they maintain necessary healthcare access during crucial times. Leveraging tools like pdfFiller not only simplifies the management of required documents but also empowers users to take control of their COBRA journey. By utilizing the resources available, you can navigate this important aspect of health coverage with confidence and ease.






For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
How can I send cobra open enrollment form for eSignature?
Can I create an electronic signature for signing my cobra open enrollment form in Gmail?
How do I complete cobra open enrollment form on an Android device?
What is cobra open enrollment form?
Who is required to file cobra open enrollment form?
How to fill out cobra open enrollment form?
What is the purpose of cobra open enrollment form?
What information must be reported on cobra open enrollment form?
pdfFiller is an end-to-end solution for managing, creating, and editing documents and forms in the cloud. Save time and hassle by preparing your tax forms online.