Get the free Submitting a Prior Authorization Request Using the AHCCCS ...
Get, Create, Make and Sign submitting a prior authorization
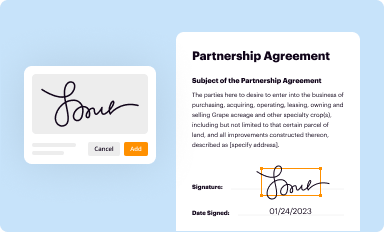
Editing submitting a prior authorization online
Uncompromising security for your PDF editing and eSignature needs
How to fill out submitting a prior authorization
How to fill out submitting a prior authorization
Who needs submitting a prior authorization?
Submitting a Prior Authorization Form: A Comprehensive Guide
Understanding prior authorization
Prior authorization is a process used by health insurance companies to determine whether they will cover a prescribed procedure or medication. This authorization is a prerequisite that healthcare clinicians must secure before providing certain healthcare services to patients. The intent behind prior authorization is to evaluate the necessity and appropriateness of a treatment or medication, ensuring it aligns with the patient's specific medical needs and the insurer's policies.
The importance of prior authorization cannot be overstated. It plays a crucial role in managing healthcare costs, helping insurers control unnecessary expenses while safeguarding patient safety. By requiring prior approval for certain treatments, insurers aim to minimize the risk of costly procedures or medications that may not provide the anticipated value. Consequently, prior authorization influences insurance coverage, determining the financial responsibility of patients and providers staff.
Key components of a prior authorization form
A complete and accurate prior authorization form is essential for ensuring timely approval. The essential information required includes patient details such as their full name, date of birth, and health insurance information. Provider information, including the prescriber's name, NPI number, and contact details, must also be included. Additionally, specific details about the procedure or medication, like CPT and HCPCS codes, need to be specified for effective processing.
In addition to basic information, supporting documentation is crucial. This may include medical records, previous treatment summaries, or diagnostic test results that substantiate the necessity of the authorization request. Providers should organize these documents systematically to ensure that gathering this information is efficient and streamlined.
The prior authorization process
Submitting a prior authorization form involves careful preparation and adherence to specific steps. First, preparation is critical. Providers should create a checklist of all necessary documents and information before beginning the submission process. This checklist acts as a roadmap, ensuring no critical component is overlooked.
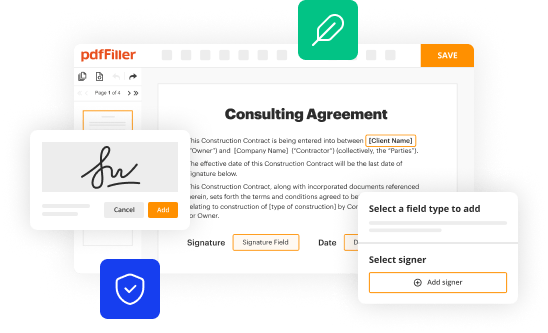
When completing the form, providers must fill in each section with precision. Reviewers at health insurance companies evaluate these forms closely, so clarity and accuracy are paramount. Lastly, understanding submission methods helps; while online portals are increasingly common, older methods such as fax and email remain viable options.
Common mistakes can derail the authorization process. Frequent errors include omitting necessary codes, providing inaccurate contact information, or submitting incomplete documentation. Ensuring that all components are in order before submission is essential to avoid delays.
Interpreting prior authorization outcomes
After submitting a prior authorization form, providers can expect a response within a specific timeframe, typically ranging from a few days to several weeks. It is essential to follow up if there is an extended silence from the insurer, as delays in these responses can impact patient care.
Understanding whether a prior authorization is approved or denied involves recognizing key criteria for approval. Health insurance companies look at the patient's clinical history, the necessity of the service, and adherence to utilization management practices. Conversely, common reasons for denial include insufficient medical justification or the lack of required documentation. If denied, providers should be prepared to gather additional information or appeal the decision.
Tips for successful prior authorization management
Healthcare providers can adopt several best practices that lead to a more efficient prior authorization workflow. First, integrating the prior authorization process into daily operations can significantly improve success rates. Encouraging staff to become familiar with frequently requested procedures and their corresponding requirements minimizes submission errors.
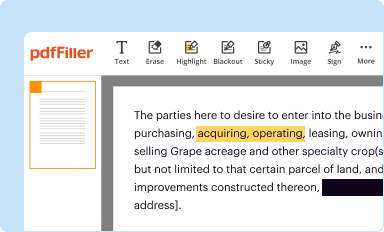
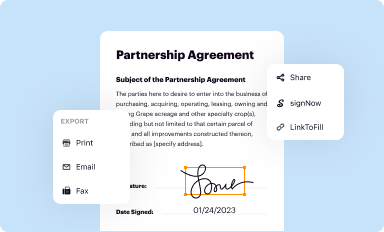
Utilizing technology, such as that offered by pdfFiller, can dramatically streamline the prior authorization process. Cloud-based solutions enable users to edit documents easily, eSign, and collaborate securely. Keeping track of submitted authorizations can also improve success rates. Utilizing tracking tools can help providers monitor the status of requests, ensuring no follow-ups fall through the cracks.
Enhancing collaboration among stakeholders
Effective communication is vital among all stakeholders in the prior authorization process. Clear channels of communication must exist between providers, insurance companies, and patients for optimal workflow. Open dialogue ensures everyone is informed about the next steps, addressing any possible issues proactively.
Patient engagement is also crucial. Providers should educate patients about the prior authorization process, explaining how it affects their care and coverage. This engagement can help alleviate patient anxiety about the process while ensuring that they understand their roles.
Future trends in prior authorization
The landscape of prior authorization is on the brink of transformation, thanks to technological innovations. New tools and software are emerging that simplify the documentation process and improve connectivity between providers and payers. Automation is becoming a common solution to reduce the burdens of manual submissions, thereby speeding up the authorization process.
In addition to these technological changes, several regulatory developments are anticipated to impact prior authorization in the coming years. Proposed healthcare laws aim to reduce barriers to care through more straightforward authorization requirements, ultimately enhancing patient access to essential services.
FAQ section
Understanding commonly asked questions about submitting a prior authorization form can help demystify the process. A common point of confusion is the difference between preauthorization and prior authorization; while they are often used interchangeably, preauthorization typically refers to the initial phase where a provider seeks approval before providing a service, whereas prior authorization may refer to any step taken after.
Another question frequently posed involves the timeline of authorization. How long does a prior authorization take? The answer can vary, but many insurance companies aim to respond within five business days. For urgent authorization requests, there are often expedited pathways available, although these typically require robust justification from the provider.
Interactive tools and resources
For those looking to efficiently manage prior authorization submissions, pdfFiller offers extensive resources. Users can access customizable prior authorization templates that simplify filling and submitting forms. Moreover, utilizing cloud-based document management ensures that critical documents are securely stored and easily accessible from any location.
Cloud-based solutions such as pdfFiller enhance the prior authorization experience by providing users with the ability to edit documents, collaborate with stakeholders, and track the submission status from one integrated platform. This level of organization and ease of use can significantly alleviate the stress associated with prior authorization submissions.






For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
How can I edit submitting a prior authorization from Google Drive?
Can I create an electronic signature for signing my submitting a prior authorization in Gmail?
How can I fill out submitting a prior authorization on an iOS device?
What is submitting a prior authorization?
Who is required to file submitting a prior authorization?
How to fill out submitting a prior authorization?
What is the purpose of submitting a prior authorization?
What information must be reported on submitting a prior authorization?
pdfFiller is an end-to-end solution for managing, creating, and editing documents and forms in the cloud. Save time and hassle by preparing your tax forms online.