Get the free PRIOR AUTHORIZATION REQUEST FORM MOUNJARO ...
Get, Create, Make and Sign prior authorization request form



Editing prior authorization request form online
Uncompromising security for your PDF editing and eSignature needs
How to fill out prior authorization request form

How to fill out prior authorization request form
Who needs prior authorization request form?
Prior Authorization Request Form - How-to Guide
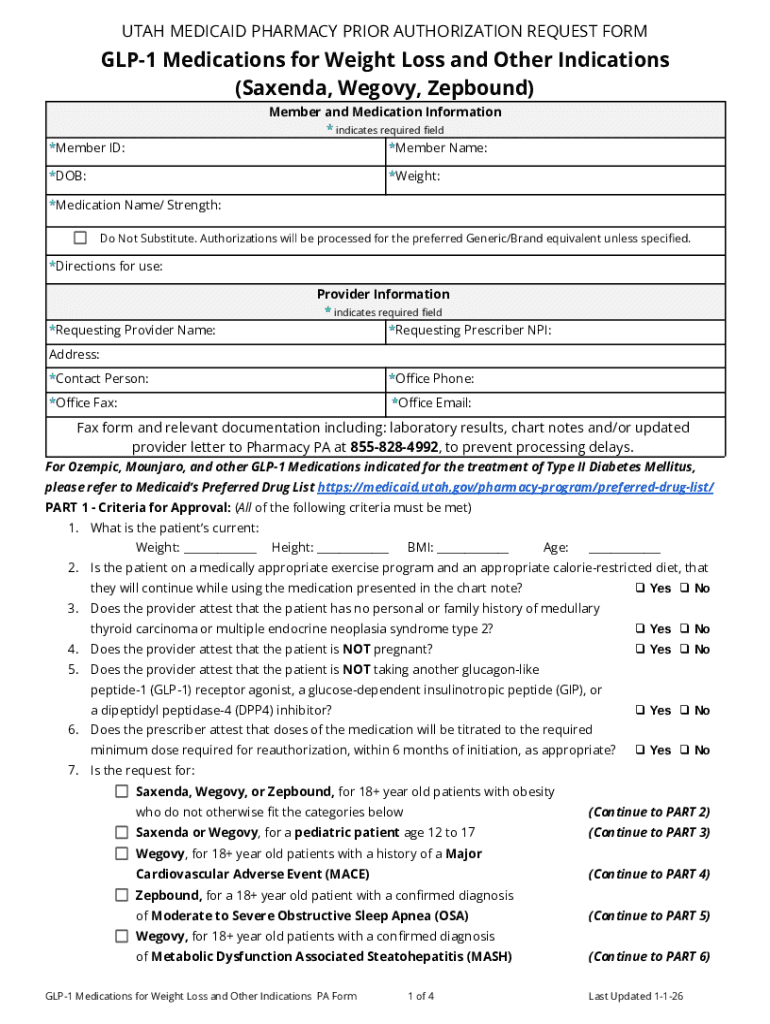
Understanding prior authorization requests
Prior authorization is a process required by many health insurance plans wherein healthcare providers must obtain approval from the payer before the patient receives certain medical services, procedures, or medications. This step ensures that the requested services are medically necessary and covered under the patient's insurance plan.
Accurate submission of prior authorization requests is critical. A well-prepared request minimizes delays in patient care and reduces the chances of a denial. The stakeholders involved in this process include healthcare providers, patients, insurance payers, and administrative support staff, all of whom must collaborate effectively to streamline the authorization process.
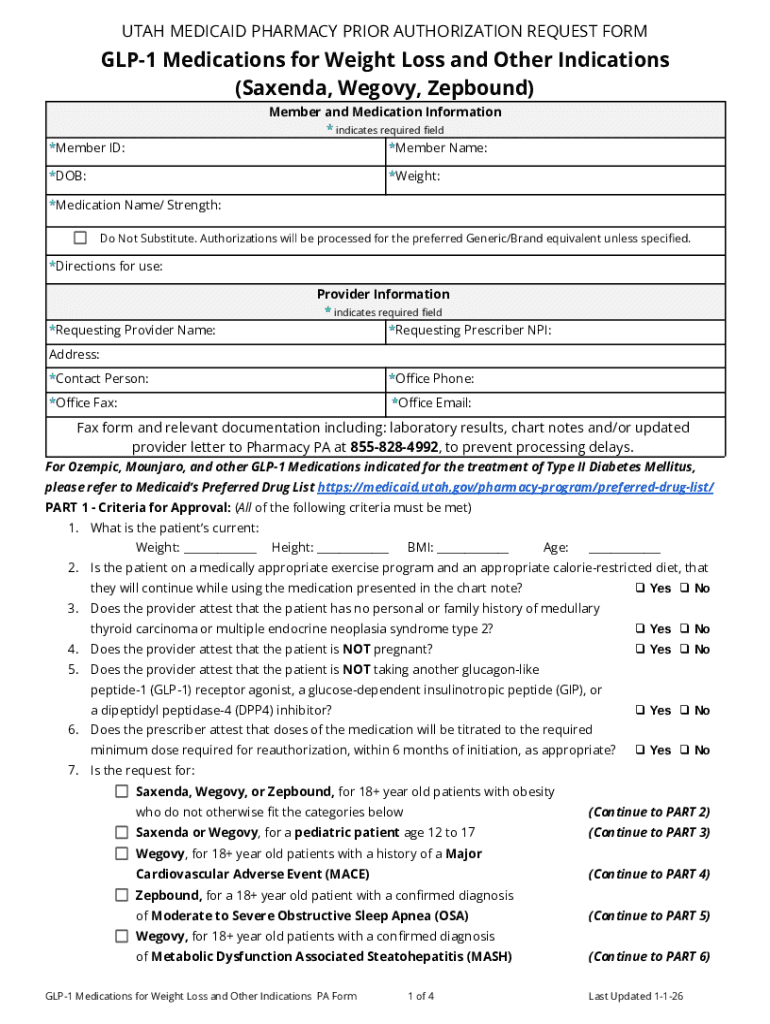
Overview of the prior authorization request form
The prior authorization request form is a document used by healthcare providers to seek approval for a patient's treatment from their insurance provider. It serves as the official request to ensure that the necessary processes are followed before a patient receives care.
Key components of the form include:
Common use cases for the form include requests for high-cost medications, specialized surgeries, and advanced imaging services.
Preparing to complete the form
Before filling out the prior authorization request form, it's essential to gather all required documentation. This includes the patient's medical records, which provide evidence of the patient's diagnosis and previous treatments, as well as supporting evidence for the requested treatment. Having complete and accurate information streamlines the process and assists in overcoming potential hurdles.
Additionally, understand that different insurance payers may have specific requirements regarding what needs to be included in the prior authorization request. Familiarizing yourself with these details ensures compliance and enhances the likelihood of approval. Utilize tools and resources such as pdfFiller to assist in document preparation.
Step-by-step guide to filling out the prior authorization request form
Filling out the prior authorization request form can initially seem daunting. However, by following these straightforward steps, healthcare providers can minimize errors and improve submission success.
Submitting the prior authorization request
Once the prior authorization request form is completed, it needs to be submitted to the appropriate insurance company for review. Healthcare providers can typically submit these requests through several methods.
Understanding the response timelines from various insurance companies is crucial. While some may respond within a few days, others might take longer. Keeping track of these timelines helps in managing follow-ups effectively.
Managing and tracking your authorization request
Once the prior authorization request has been submitted, tracking the submission becomes essential. This step ensures that you're aware of any responses from payers promptly.
It's important to follow up with payers if you haven't heard back within the expected timeframe. Utilize tools designed for monitoring authorization statuses, such as pdfFiller's tracking features, which can simplify and expedite the process.
Common challenges and how to overcome them
Navigating the prior authorization process can lead to challenges, especially in the case of denials. Should a request be denied, understanding the reasons behind the denial and having a clear follow-up procedure can facilitate getting the authorization successfully.
Assessing feedback and adjusting submissions accordingly is critical. If necessary, prepare for the appeals process, which allows you to contest a denial and provide additional supporting documentation.
Best practices for efficient prior authorization management
Implementing best practices in managing prior authorization requests can significantly enhance operational efficiency. One effective strategy is utilizing technology to create templates and document formats that streamline the process.
Moreover, collaboration with your team is vital for ensuring a seamless workflow, and continuous training on any changes in the authorization process can prevent setbacks. These best practices ultimately lead to improved patient care and satisfaction.
Frequently asked questions (FAQs)
Prior authorization requests can prompt several questions, including:
Additional support and resources
For those seeking further assistance, accessing sample prior authorization forms can provide valuable templates. Additionally, checking links to payer-specific requirements can give insight into what each insurance provider needs.
Engaging with community forums focused on prior authorization processes can also be beneficial for sharing tips and best practices with other healthcare professionals.






For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
How can I edit prior authorization request form from Google Drive?
How do I edit prior authorization request form in Chrome?
How do I complete prior authorization request form on an iOS device?
What is prior authorization request form?
Who is required to file prior authorization request form?
How to fill out prior authorization request form?
What is the purpose of prior authorization request form?
What information must be reported on prior authorization request form?
pdfFiller is an end-to-end solution for managing, creating, and editing documents and forms in the cloud. Save time and hassle by preparing your tax forms online.