Get the free Request a Coverage DecisionAetna Medicare
Get, Create, Make and Sign request a coverage decisionaetna



Editing request a coverage decisionaetna online
Uncompromising security for your PDF editing and eSignature needs
How to fill out request a coverage decisionaetna

How to fill out request a coverage decisionaetna
Who needs request a coverage decisionaetna?
Request a Coverage Decision Aetna Form: A Comprehensive Guide
Overview of coverage decisions
Coverage decisions are determinations made by insurance providers regarding whether a specific treatment, service, or procedure will be covered under a health insurance plan. These decisions are crucial because they directly impact the availability of essential medical care for members.
Understanding the nuances of coverage processes can empower members to navigate their healthcare options more effectively. Aetna is a prominent provider in the health insurance space, offering a variety of policies. Familiarizing yourself with their coverage policies is vital for ensuring you receive the care you need without unexpected costs.
When to request a coverage decision
There are specific situations where requesting a coverage decision may be necessary. For instance, when a new treatment plan or procedure is being considered, it is wise to confirm whether Aetna will cover it.
Similarly, if there is a change in a current treatment or if a claim for services has been denied, seeking a coverage decision becomes critical. Members should also be well-versed in their policy exclusions and limitations, as these can affect the eligibility of certain treatments or services.
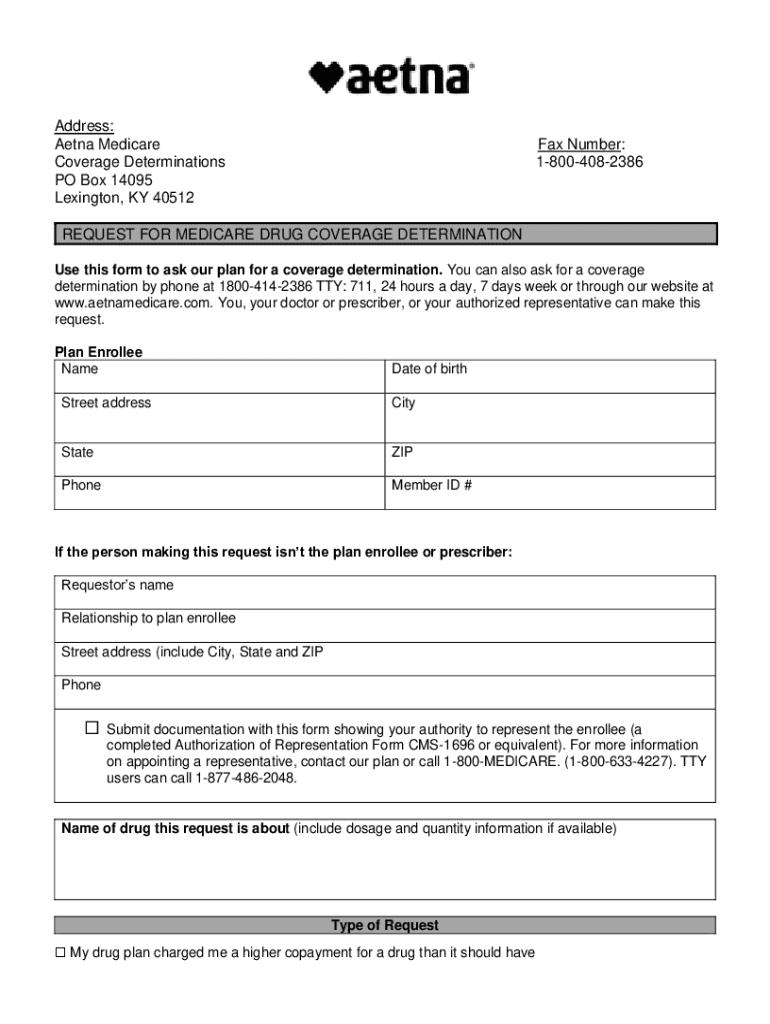
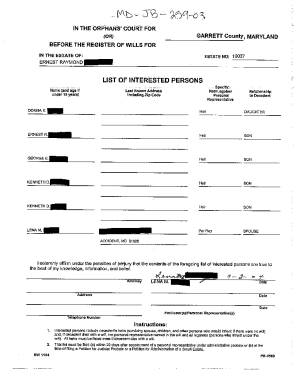
Key components of the Aetna coverage decision request form
The Aetna coverage decision request form is a crucial tool for members seeking clarity on coverage. This form captures all essential information needed to assess the request. Applicants should complete this form as accurately and comprehensively as possible.
Essential details include the insured's information, the provider's information, and a clear description of the requested coverage. By using this form effectively, members can improve their chances of obtaining the desired coverage.
Step-by-step guide to filling out the Aetna coverage decision form
Filling out the Aetna coverage decision form requires attention to detail. Here’s a structured approach to ensure a smooth submission process.
Submitting the coverage decision request
Once the Aetna coverage decision form is completed, it needs to be submitted. Aetna offers multiple submission methods to facilitate this process.
You can submit your request online through Aetna's portal, or you can choose to fax or mail it. The online submission process is typically the quickest way to submit your request. After submission, tracking the status of your request is essential to know when to expect a response.
Common reasons for coverage decision denials
Not every request for coverage will be approved. Members should understand typical scenarios that may lead to denials. Familiarizing oneself with Aetna's coverage policies can shed light on why certain requests may be turned down.
Common reasons include lack of medical necessity, treatments falling under exclusions, or insufficient evidence supporting the need for the service. Being aware of these potential pitfalls can prepare members for addressing and responding to denials effectively.
Appeal process for unfavorable coverage decisions
If a coverage decision is unfavorable, members have the right to appeal. Understanding Aetna's appeal process is crucial for those looking to challenge a denial. Typically, there are specific timeframes within which you must submit an appeal.
Gathering the required documentation for appeals is essential. Including any additional evidence that supports the necessity of the treatment can significantly bolster the chances of a successful appeal. Here are some tips to navigate the appeal process.
Additional support resources
Members can access numerous resources when navigating coverage decisions. Contacting Aetna directly can provide clarity and resolution for any concerns. Aetna offers customer service numbers and online chat options for immediate assistance.
Additionally, healthcare providers can often assist in navigating the coverage decision process. Advocacy groups and community resources may also provide support to ensure that members understand their rights and options.
Frequently asked questions (faqs)
As members prepare to request a coverage decision with Aetna, they often have common queries that can help clarify the process. Addressing these FAQs can remove confusion and streamline the experience.
Interactive tools for users
Utilizing interactive tools can enhance the experience of requesting a coverage decision. Document management tools, such as those available on pdfFiller, offer users the ability to edit, sign, collaborate, and manage their forms in one central location.
By using pdfFiller's features, you can access Aetna forms, customize documents for specific needs, and streamline the overall submission process.
Final thoughts on navigating coverage decisions with Aetna
In summary, understanding the process of requesting coverage decisions from Aetna is essential for accessing necessary healthcare services. By harnessing the power of the Aetna coverage decision request form and utilizing resources provided through platforms like pdfFiller, users can navigate this complex landscape more effectively.
Empowering yourself with the right tools and knowledge ensures you can advocate for your healthcare needs. Whether it’s submitting a request or appealing a denial, being well-prepared and informed is the key to success.






For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
How can I modify request a coverage decisionaetna without leaving Google Drive?
How do I make changes in request a coverage decisionaetna?
How can I fill out request a coverage decisionaetna on an iOS device?
What is request a coverage decisionaetna?
Who is required to file request a coverage decisionaetna?
How to fill out request a coverage decisionaetna?
What is the purpose of request a coverage decisionaetna?
What information must be reported on request a coverage decisionaetna?
pdfFiller is an end-to-end solution for managing, creating, and editing documents and forms in the cloud. Save time and hassle by preparing your tax forms online.