Get the free Geriatric Suicide in Primary Care: A Fact SheetACU
Get, Create, Make and Sign geriatric suicide in primary



Editing geriatric suicide in primary online
Uncompromising security for your PDF editing and eSignature needs
How to fill out geriatric suicide in primary

How to fill out geriatric suicide in primary
Who needs geriatric suicide in primary?
Geriatric suicide in primary form
Understanding geriatric suicide
Geriatric suicide represents a poignant issue in mental health, focusing on self-inflicted death among older adults. Defined as suicides within the senior demographic, it reflects a tragic facet of societal challenges related to aging, requiring immediate attention and intervention.
Statistics indicate that individuals aged 65 and older have the highest suicide rates compared to other age groups. Studies reveal that factors such as mental health disorders, chronic illnesses, and various life transitions significantly contribute to this disturbing trend. Societal perceptions often stigmatize mental health discussions within this demographic, creating barriers to seeking help.
Contributing factors
Geriatric suicide often stems from a combination of mental health disorders prevalent in older adults, including depression and anxiety. These conditions may be exacerbated by cognitive impairments, which further complicate emotional wellness. It's crucial to recognize that the mental health of older adults can be significantly affected by various physical health issues, such as chronic illnesses, which contribute to feelings of hopelessness.
Major life transitions, such as retirement, the death of loved ones, and social isolation, can severely impact mental well-being. The loss of purpose following retirement can trigger significant psychological distress, while bereavement can lead to profound grief, contributing to suicidal ideation.
Warning signs of geriatric suicide
Recognizing the warning signs of suicidal ideation in older adults is vital. Sudden changes in behavior or mood, withdrawal from previous interests, and a noticeable decline in social engagement can be critical indicators. Conversations expressing feelings of hopelessness or stating they feel like a burden must be taken seriously.
Verbal cues can often illuminate an individual’s emotional state. Phrases indicating despair or a lack of future hope should prompt immediate concern. Moreover, physical signs, such as neglecting personal hygiene or drastic changes in eating and sleeping patterns, are equally alarming and should be addressed promptly.
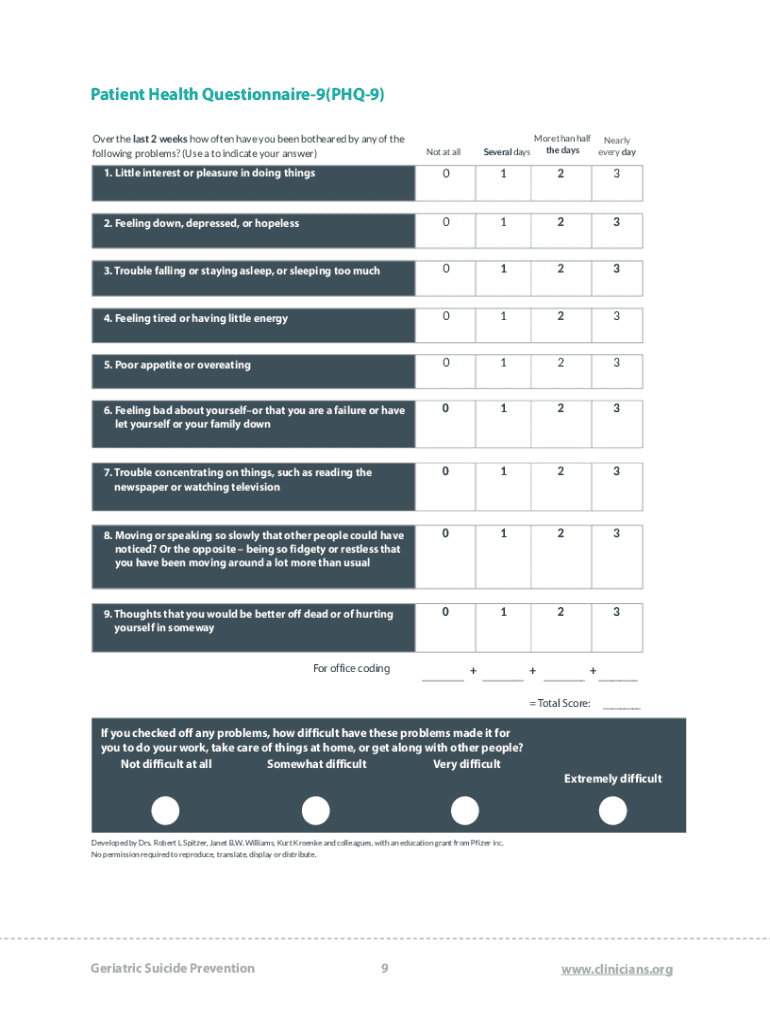
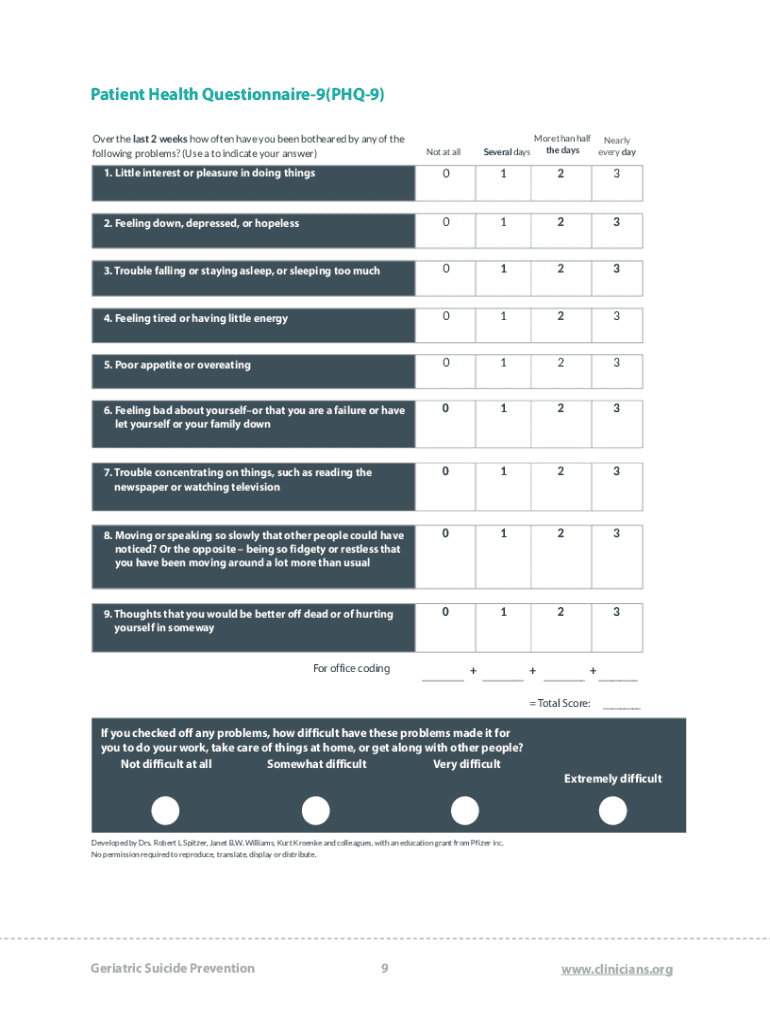
Primary care's role in identifying risks
Primary care providers play a crucial role in identifying and mitigating risks of geriatric suicide. Incorporating routine mental health screenings into regular health assessments can facilitate early detection. Using validated tools like the Geriatric Depression Scale or Beck Depression Inventory allows for more structured evaluations of mental health.
Discussion techniques are also imperative in building rapport and encouraging older patients to express their feelings openly. Approaching these conversations with empathy and kindness, along with employing open-ended questions, can foster a safer environment to discuss mental health concerns.
Interventions and support options
When confronting potential suicidality, immediate safety measures are essential. Creating a comprehensive safety plan tailored to the individual can provide them with immediate resources and an actionable roadmap during crises. This can include emergency contact numbers and mental health support services.
In addition, therapeutic approaches such as Cognitive Behavioral Therapy (CBT) have shown efficacy in addressing cognitive distortions prevalent in older adults. Group therapy can also provide much-needed social support, as shared experiences among peers can reduce feelings of isolation.
Creating a supportive environment
Building a supportive environment for older adults is essential in preventing isolation and loneliness, which are direct contributors to geriatric suicide. Encouraging engagement in community activities or clubs fosters connections that are crucial for emotional support. Connection enhances not only wellness but also reinforces independence and empowerment.
Tailored health care programs focusing on geriatric needs offer a holistic approach, incorporating both physical and mental health services. Innovative models of care that look beyond traditional healthcare solutions can transform geriatric care, addressing the multifaceted challenges faced by this population.
Legal and ethical considerations in care
Navigating legal and ethical considerations when caring for the elder population is complex, particularly regarding consent and capacity. Understanding the legal frameworks surrounding treatment can guide healthcare providers in ensuring that the rights and preferences of older adults are respected throughout their care.
Moreover, facilitating end-of-life discussions with sensitivity is paramount. Advance care planning allows individuals to express their wishes in response to potential crises, thereby offering them dignity and control over their treatment options.
Specific resources for care providers
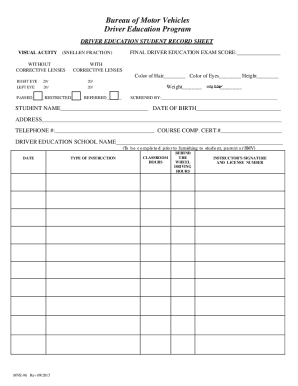
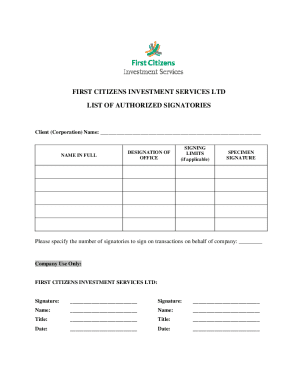
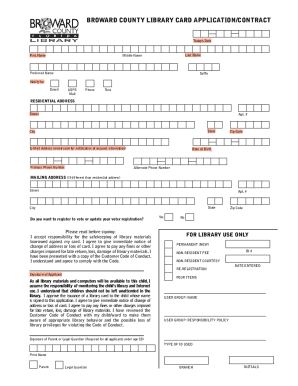
Healthcare professionals should be equipped with the right tools and resources to engage effectively with elder patients. Comprehensive toolkits and guides offer valuable insights into recognizing the warning signs of increasing suicidality, along with practical steps for intervention. Interactive templates for documentation can streamline the assessment process, making it easier for caregivers.
Training programs dedicated to geriatric mental health encourage ongoing education, thus empowering healthcare professionals to stay informed and effective. Workshops can cover a spectrum of topics, enhancing the skills required to support elderly patients in navigating mental health challenges.
Community and online support resources
Access to appropriate support resources is crucial for older adults facing mental health challenges. National and local helplines provide immediate assistance and should be readily accessible to families and individuals. Engaging with local community services can enhance connections for seniors, helping to alleviate the feelings of loneliness.
Additionally, numerous online platforms offer seminars, articles, and discussions about geriatric mental health. These resources serve as educational hubs for both practitioners and families seeking to understand and assist elderly individuals better.
Innovative solutions for geriatric mental health
Integrating technology into geriatric mental health care is an emerging solution that can significantly enhance outcomes. Digital tools and applications aimed at promoting mental wellness among older adults provide unique opportunities for engagement and interaction. For instance, mindfulness apps and online support groups can create nurturing environments that foster connection.
Looking ahead, the future of geriatric care must adapt to the evolving needs of the elderly population. Innovative care models, emphasizing a multidisciplinary approach, are essential. By combining healthcare professionals from various fields, we can create a more comprehensive support system that addresses both physical and mental health.






For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
How do I make changes in geriatric suicide in primary?
Can I create an electronic signature for signing my geriatric suicide in primary in Gmail?
How do I complete geriatric suicide in primary on an iOS device?
What is geriatric suicide in primary?
Who is required to file geriatric suicide in primary?
How to fill out geriatric suicide in primary?
What is the purpose of geriatric suicide in primary?
What information must be reported on geriatric suicide in primary?
pdfFiller is an end-to-end solution for managing, creating, and editing documents and forms in the cloud. Save time and hassle by preparing your tax forms online.