Get the free colorado standard prior authorization request form- sud ...
Get, Create, Make and Sign colorado standard prior authorization



How to edit colorado standard prior authorization online
Uncompromising security for your PDF editing and eSignature needs
How to fill out colorado standard prior authorization

How to fill out colorado standard prior authorization
Who needs colorado standard prior authorization?
Understanding the Colorado Standard Prior Authorization Form
Overview of the Colorado Standard Prior Authorization Form
The Colorado Standard Prior Authorization Form is a standardized document used across the state to streamline the process of obtaining prior authorization for healthcare services. By consolidating requests into one format, this form ensures that healthcare providers, patients, and insurers are all aligned on the necessary details for medical treatment approval.
This form serves multiple purposes: primarily, it is designed to facilitate communication between healthcare providers and insurance companies, ensuring that all required information is provided upfront. It plays a crucial role in the healthcare ecosystem, particularly as it helps manage costs, maintains a level of care, and reduces unnecessary treatments.
Who needs the Colorado Standard Prior Authorization Form?
The Colorado Standard Prior Authorization Form is essential for various stakeholders within the healthcare system. Healthcare providers, including physicians, specialists, and various medical facilities like hospitals and clinics, rely heavily on this form to gain authorization for treatments that may not be covered under patients' insurance plans without prior approval.
Patients and their families also play a crucial role in the authorization process. It is vital they understand their rights and responsibilities when interacting with their insurers, especially regarding what services might require prior authorization. Lastly, insurance companies utilize this form to evaluate and determine the necessity and appropriateness of requested services before approving claims.
Detailed breakdown of the standard form
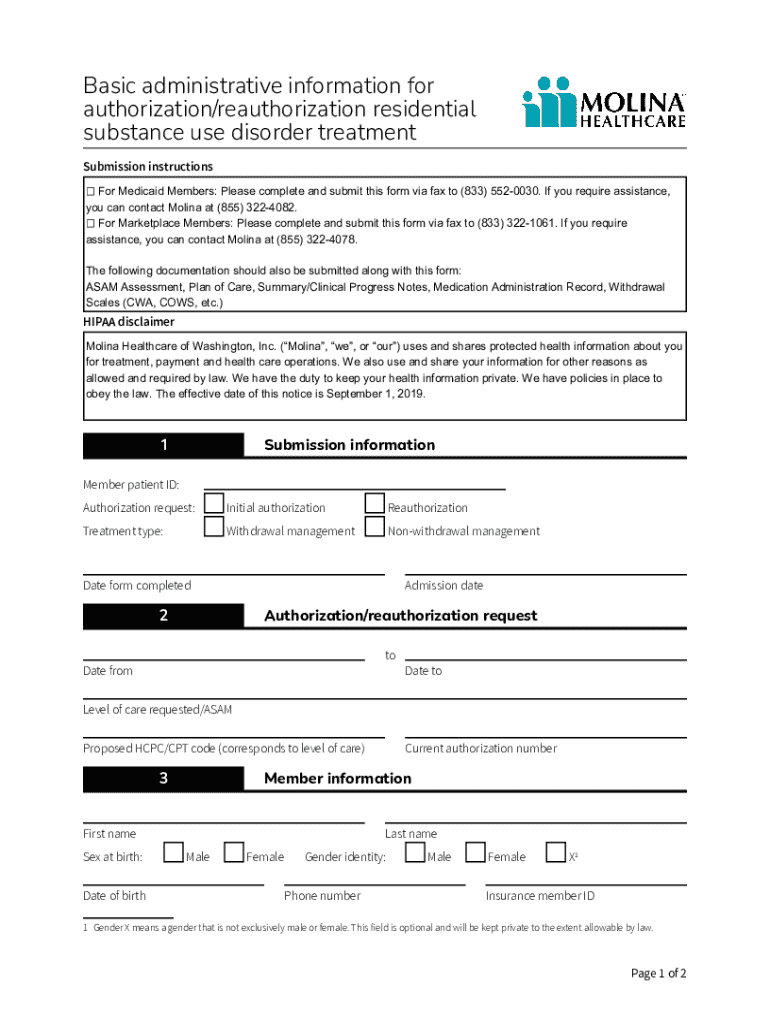
The Colorado Standard Prior Authorization Form is organized into distinct sections, each designed to collect specific information essential for processing the authorization request efficiently. The main sections include Patient Information, Provider Information, and the Procedure or Service Requested.
Filling out the Patient Information section requires details such as the patient’s name, date of birth, insurance information, and contact details. The Provider Information section should include the provider's name, practice address, NPI number, and any other relevant credentials. In the Procedure or Service Requested section, a clear description of the requested treatment or service, along with justifications for its necessity, must be included. Accurate data in this area can significantly influence the approval outcome.
Step-by-step guide to completing the form
Completing the Colorado Standard Prior Authorization Form can seem daunting, but breaking it down into manageable steps can ease the process. Start by gathering all necessary information and documents, including any previous medical records or test results that support the necessity of the treatment.
After gathering the required data, proceed to fill out the form. Be mindful of the instructions provided for each section to ensure accuracy. Once completed, submit the form through one of the accepted submission methods, which include online, mail, or fax. After submission, it’s important to follow up on your request to check the status of the authorization.
Common challenges and solutions
Despite its standardization, users may encounter challenges while using the Colorado Standard Prior Authorization Form. Common errors include missing information, incorrect coding, or misunderstandings about what justifications are necessary. These mistakes can delay the authorization process or lead to denials.
To resolve issues that arise, contacting insurance representatives for clarification on denials or submission errors is a prudent first step. If an authorization request is denied, patients have the right to appeal the decision, which requires detailed justification and engagement with the insurer.
Utilizing pdfFiller for efficient form management
pdfFiller offers an efficient way to manage the Colorado Standard Prior Authorization Form. One of the biggest advantages of using pdfFiller is the ability to edit documents in a cloud-based environment. This enables healthcare providers, patients, and administrators to access the form from any device, anywhere, ensuring that they can complete and submit authorization requests without being tied to a specific location.
In addition to ease of access, pdfFiller provides real-time collaboration tools that allow multiple users to contribute to form completion. Users can easily upload the Colorado Standard Prior Authorization Form into pdfFiller, edit it directly, fill it out, eSign, and send it for approval in just a few quick steps. This simplifies the entire process and minimizes delays.
Frequently asked questions about the Colorado Standard Prior Authorization Form
Many users have common questions regarding the Colorado Standard Prior Authorization Form that reflect concerns about its use and implications. One frequent question pertains to the duration of the authorization process, which can vary significantly based on the insurer—ranging from a few hours to several days.
Another prevalent question is what happens if a request is denied. Patients have the right to understand the reasons for denial and may need to provide additional evidence or follow the appeal process. Clarifying these aspects is essential for both patients and healthcare providers to navigate the complexities of insurance authorizations.
Related forms and templates
The Colorado Standard Prior Authorization Form is part of a broader landscape of healthcare documentation and authorization processes. There are other key forms and templates that relate closely to the authorization process, such as Care Coordination Referral Forms and Claims Submission Forms. Understanding these related forms helps patients and providers manage documentation more effectively.
Integrating these forms with the prior authorization process not only improves the efficiency of healthcare delivery but also minimizes the likelihood of errors or delays. Each form plays a role in ensuring that patients receive timely care while keeping insurers informed about the patient's treatment journey.
Popular searches related to prior authorization
Individuals searching for the Colorado Standard Prior Authorization Form often explore related terms and concepts as well. Key searches may include topics like Utilization Management and Pharmacy and Medication Approvals, as these areas frequently intersect with the authorization process.
Resources designed to assist healthcare providers and patients can significantly enhance the user experience. Having access to tools and information that simplify the prior authorization process ultimately benefits everyone involved, providing a clearer pathway to ensure patients receive necessary medical attention without unnecessary delays.






For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
Where do I find colorado standard prior authorization?
Can I create an electronic signature for signing my colorado standard prior authorization in Gmail?
How do I complete colorado standard prior authorization on an Android device?
What is colorado standard prior authorization?
Who is required to file colorado standard prior authorization?
How to fill out colorado standard prior authorization?
What is the purpose of colorado standard prior authorization?
What information must be reported on colorado standard prior authorization?
pdfFiller is an end-to-end solution for managing, creating, and editing documents and forms in the cloud. Save time and hassle by preparing your tax forms online.