Get the free Prime-Prior-Authorization-Request-Form.docx
Get, Create, Make and Sign prime-prior-authorization-request-formdocx



How to edit prime-prior-authorization-request-formdocx online
Uncompromising security for your PDF editing and eSignature needs
How to fill out prime-prior-authorization-request-formdocx

How to fill out prime-prior-authorization-request-formdocx
Who needs prime-prior-authorization-request-formdocx?
Comprehensive Guide to the Prime Prior Authorization Request Form
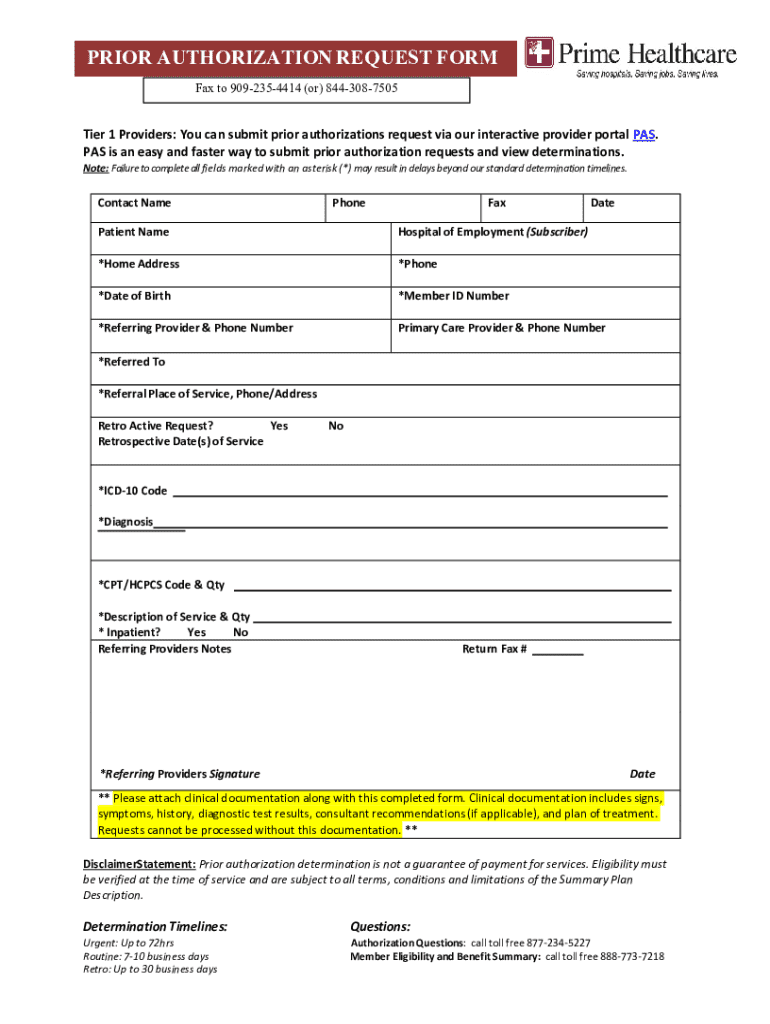
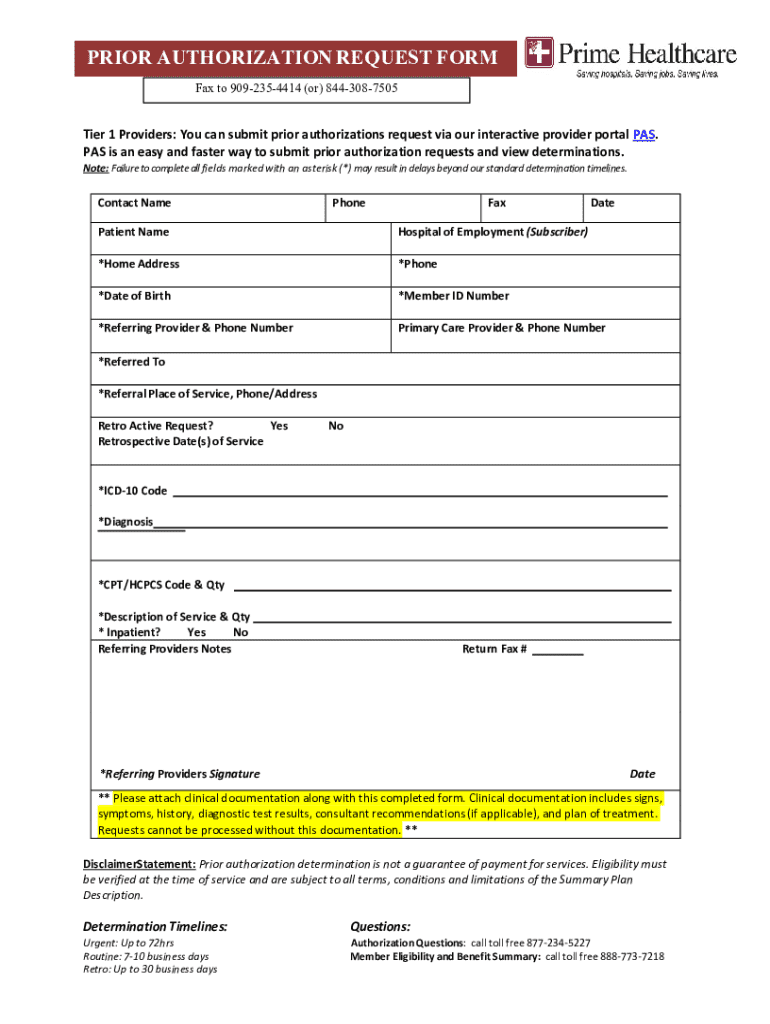
Understanding the Prime Prior Authorization Request Form
Prior authorization is a process utilized by healthcare insurers to determine if they will cover a prescribed service, treatment, or medication. This step is crucial as it safeguards against unnecessary costs and ensures that proposed medical interventions are appropriate for the patient's condition. In many cases, particularly for high-cost procedures or specialty drugs, prior authorization is a necessary hurdle for both providers and patients.
The Prime Prior Authorization Request Form specifically caters to these needs, providing a structured method for healthcare providers to request prior authorization from insurance companies. It is vital for services like surgeries, certain diagnostic tests, imaging services, and costly medications that insurers want to evaluate before agreeing to coverage.
Key components of the Prime Prior Authorization Request Form
The design of the Prime Prior Authorization Request Form is user-oriented and well-sectioned to streamline the submission process. Understanding its structure is essential for both healthcare providers and patients to facilitate clarity and accuracy in requests.
The form typically includes several sections, each requiring specific information: patient details, provider information, and specifics about the medical services requested. Each field is intentionally placed to minimize errors and ensure all essential information is collected.
How to fill out the Prime Prior Authorization Request Form
Filling out the Prime Prior Authorization Request Form correctly is crucial to ensure timely approval for necessary medical services. Here is a step-by-step guide for completion.
Step 1 is to gather all required information. Collect documents that have the patient's medical history, relating diagnoses, CPT codes for requested services, and any other relevant medical information.
In Step 2, carefully fill in the patient information section, ensuring that each detail matches official documents to avoid processing delays. In Step 3, input accurate provider details, confirming that the NPI is correct to prevent further issues.
Finally, Step 4 involves specifying the requested services. Use official CPT and diagnosis codes to provide clarity—this precision can significantly influence approval chances.
Editing and managing your completed form
Once the form is completed, using pdfFiller tools to edit is straightforward. Users can upload the Prime Prior Authorization Request Form to the platform, enabling them to modify any part of the document in real-time.
With pdfFiller’s features, such as text editing and image insertion, making last-minute adjustments is convenient and ensures that the form meets the necessary standards before submission.
Additionally, pdfFiller provides a seamless eSigning process. This allows providers to electronically sign the document, ensuring compliance with legal standards while saving time.
Submitting the Prime Prior Authorization Request Form
Understanding the submission process is equally important as filling out the form. There are several methods to deliver the Prime Prior Authorization Request Form to insurance companies: by fax, email, or online portals. Each method requires specific documentation to complete.
After submission, tracking the request is essential. You can confirm receipt by following up through the submission method used. Establishing communication with the insurance company's representative can facilitate prompt updates on the approval process.
Common challenges and solutions
Despite following procedures closely, approval issues may occur. Common denial reasons often include incomplete information, lack of medical necessity, or discrepancies in patient data. Addressing these challenges requires proper documentation to support the request.
If you encounter a denial, assessing the rejection reason is key. Gather additional supporting documentation, such as clinical notes or prior medical history, to build a strong case during the appeal process. Engaging with an insurance advocate may also be beneficial.
Interactive tools and resources offered by pdfFiller
Collaboration is crucial in managing prior authorization requests, especially for teams. With pdfFiller, real-time collaboration features enable multiple team members to work on the Prime Prior Authorization Request Form concurrently.
Moreover, pdfFiller offers access to a broad range of templates for other necessary healthcare forms. This centralized platform streamlines document management, making compliance and record-keeping significantly easier.
Tips for teams handling multiple requests
For healthcare teams facing multiple prior authorization requests, efficiency is paramount. Implementing strategies to manage these requests can significantly reduce workload and improve response times.
Utilizing pdfFiller’s cloud-based management system allows team members to access and update documents from any location. This supports a dynamic workflow, fostering better communication and collaboration among colleagues.
FAQs about the Prime Prior Authorization Request Form
As you engage with the Prime Prior Authorization Request Form, you may encounter questions regarding its filling process and submission guidelines. Below are responses to some commonly asked questions.






For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
How can I get prime-prior-authorization-request-formdocx?
How do I make edits in prime-prior-authorization-request-formdocx without leaving Chrome?
How do I edit prime-prior-authorization-request-formdocx on an Android device?
What is prime-prior-authorization-request-formdocx?
Who is required to file prime-prior-authorization-request-formdocx?
How to fill out prime-prior-authorization-request-formdocx?
What is the purpose of prime-prior-authorization-request-formdocx?
What information must be reported on prime-prior-authorization-request-formdocx?
pdfFiller is an end-to-end solution for managing, creating, and editing documents and forms in the cloud. Save time and hassle by preparing your tax forms online.