Get the free ca PRIOR TO ORDERING THIS
Get, Create, Make and Sign ca prior to ordering
Editing ca prior to ordering online
Uncompromising security for your PDF editing and eSignature needs
How to fill out ca prior to ordering
How to fill out ca prior to ordering
Who needs ca prior to ordering?
Navigating the CA Prior to Ordering Form: A Comprehensive Guide
Overview of prior authorization in California
Prior authorization is a crucial step in the healthcare process in California, aimed at ensuring that patients receive medically necessary care. This process involves obtaining approval from a patient's health insurance provider before a service or medication is administered. Essentially, it acts as a safety net that confirms the appropriateness of care before it is delivered, which is vital in managing both patient health and healthcare costs. Without this mechanism in place, insurance companies risk covering services that may not be necessary or effective.
The importance of prior authorization cannot be overstated. It safeguards patients by confirming that the proposed treatment is suitable based on clinical guidelines. In doing so, prior authorization protects patients from potential harm caused by inappropriate interventions and plays a significant role in controlling healthcare expenditures. By ensuring that only necessary therapies are approved, insurance providers can manage costs more effectively, contributing to the sustainability of healthcare systems. This balance of care and cost management is crucial in today’s healthcare landscape.
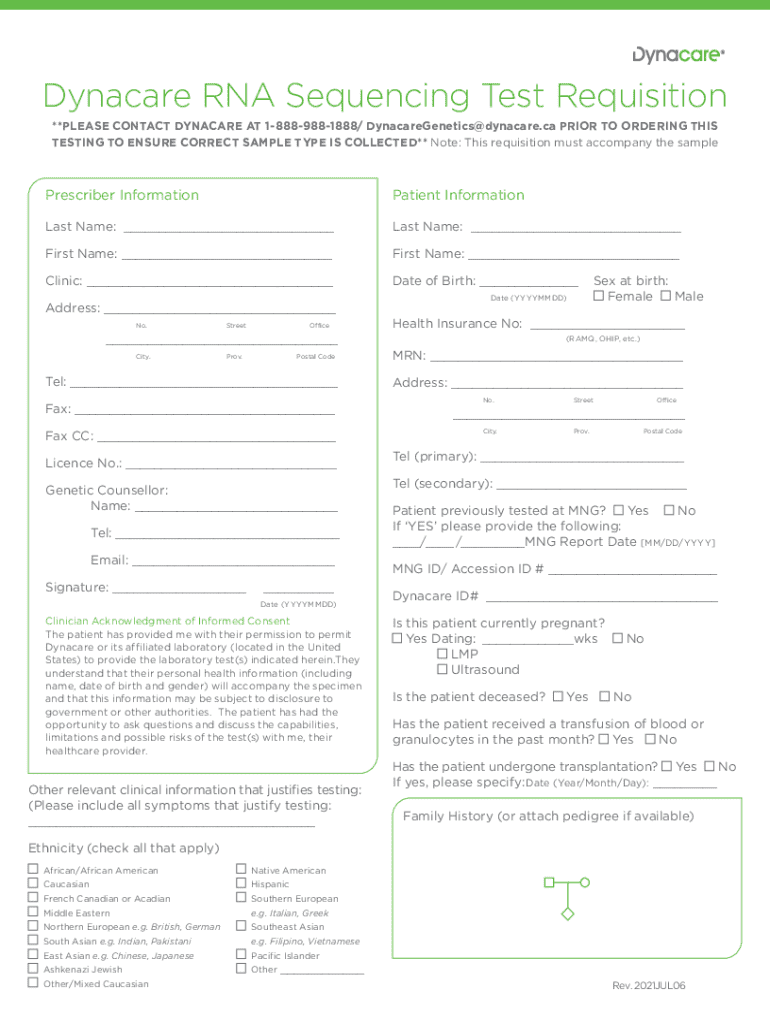
Understanding the CA prior to ordering form
The CA Prior to Ordering Form is specifically designed for healthcare providers in California to request authorization for various medical services and medications. The form streamlines the prior authorization process by consolidating all necessary information into a single document that is submitted to the appropriate insurance provider. This clarity helps minimize delays that often occur in care delivery while ensuring compliance with insurance guidelines.
Common scenarios requiring the CA Prior to Ordering Form include procedures such as surgeries, advanced imaging (like MRIs or CT scans), and specialty medications not on a standard formulary. For instance, if a physician prescribes a new medication for a chronic condition that stands outside the usual treatment protocols, completing this form becomes essential. The proactive nature of the CA Prior to Ordering Form helps healthcare providers secure timely and necessary approvals, ultimately supporting patient outcomes.
Key components of the CA prior to ordering form
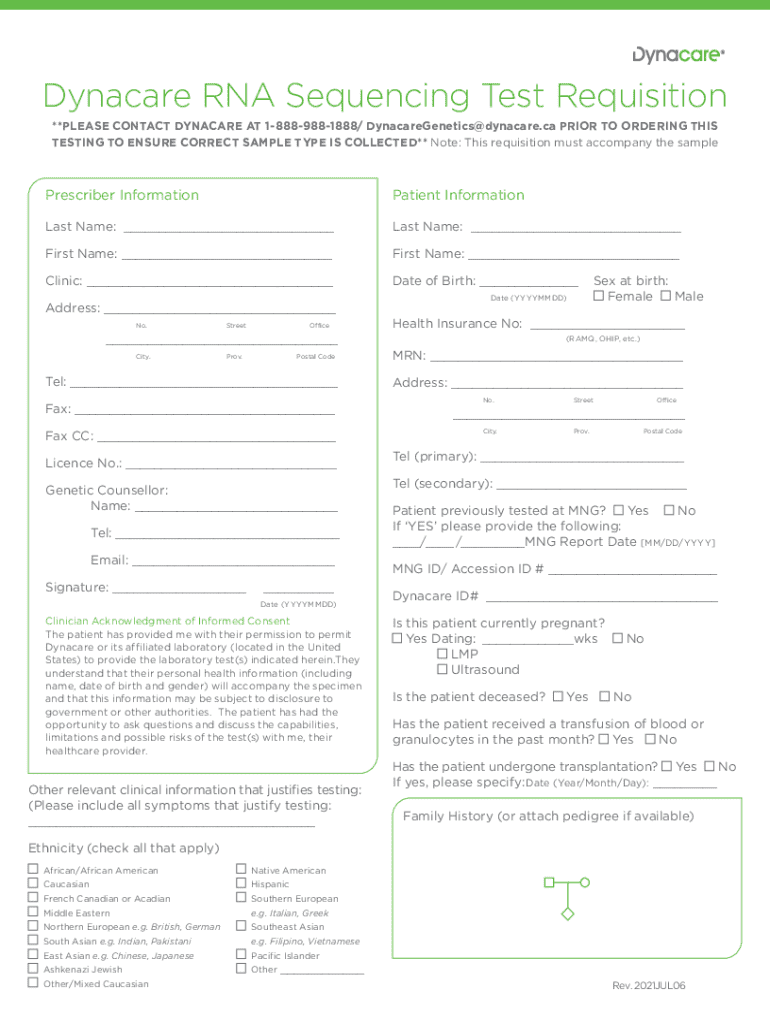
The CA Prior to Ordering Form features several key components that facilitate its effective use. Each section plays a specific role in gathering essential information required for approval. The patient information section typically includes crucial details such as the patient's name, date of birth, and insurance information. Providing accurate data in this section is imperative to avoid any miscommunication or errors that could delay the authorization.
Additionally, the provider information section requests details about the healthcare provider, including their name, contact information, and National Provider Identifier (NPI) number. This ensures that the insurance company can easily identify and communicate with the provider. The service or medication requested must be clearly described, with specific attention to any relevant clinical details. Supporting documentation is also vital; it may include clinical notes and diagnostic codes to strengthen the authorization request. These components, when filled accurately, increase the likelihood of a swift approval process.
Step-by-step guide to completing the CA prior to ordering form
Completing the CA Prior to Ordering Form requires careful attention to detail. Start with gathering all necessary information related to both the patient and the healthcare provider. This includes confirming the patient's insurance coverage to ensure that the right plan is being considered for the request. Collect insights about the patient's medical history relevant to the requested service, as this will aid in filling out the form accurately.
Next, proceed to fill out each section of the form systematically. When detailing the service or medication requested, provide as much specificity as possible, including dosage and treatment duration. Common pitfalls include omitting required fields; thus, it is essential to double-check each section before moving on. After completing the form, compile the supporting documents typically needed, such as prior clinical notes, lab results, or imaging reports that substantiate the necessity of the request.
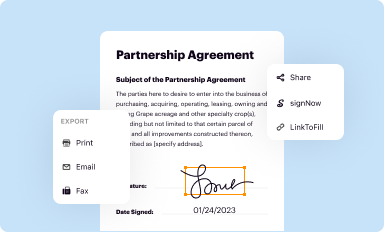
The submission phase can vary based on the insurance provider's guidelines. For some, electronic submission might be preferred, allowing healthcare teams to receive faster processing times. In contrast, others may require a paper form to be mailed. Always follow the specific submission instructions provided by the insurance company to avoid complications.
Tracking your prior authorization request
Once the CA Prior to Ordering Form is submitted, understanding the timelines for approval is crucial. Typically, insurance providers adhere to a standard review period, which can range from a few business days to up to 14 days for a routine authorization. Urgent requests may warrant expedited review, often requiring a response within 72 hours, depending on the urgency of the medical situation involved.
To follow up on your request, it's advisable to contact the insurance company's prior authorization department directly. Maintaining an organized record of your submission, including the date sent and any reference numbers, will assist with these inquiries. If a prior authorization request is denied, understanding the reasons for denial is key. Common reasons include lack of medical necessity or missing documentation. In such cases, providers can appeal the denial by addressing each point raised by the insurer and providing additional documentation or clarification.
Tips for successful prior authorizations
Accuracy and completeness are paramount in the prior authorization process. Double-checking the provided information can prevent unnecessary delays and resulting logistical issues. Additionally, open communication among providers, patients, and the insurance company plays a vital role in a smooth authorization process. Keeping all parties informed contributes to a faster resolution and adherence to necessary protocols.
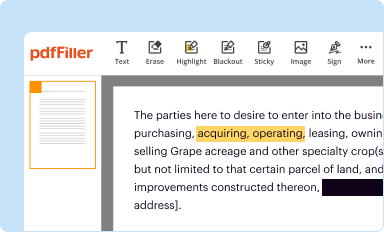
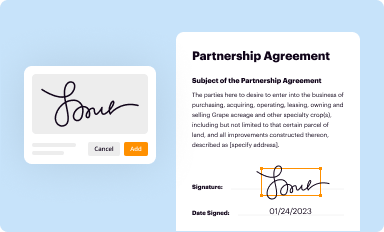
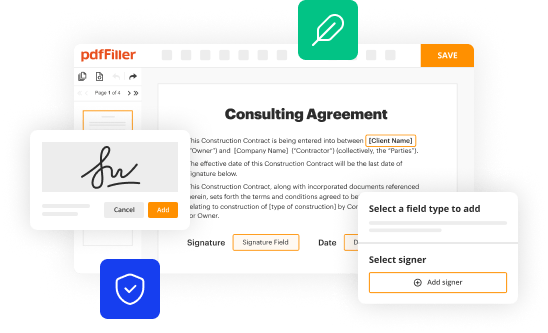
Utilizing digital tools can further streamline this process. Platforms like pdfFiller offer user-friendly features that empower providers to fill forms, edit PDFs, eSign documents, and store files in the cloud seamlessly. This simplifies the task of managing multiple documents associated with prior authorizations, allowing users to access records from any location effortlessly. Adopting digital solutions not only saves time but also enhances accuracy throughout the documentation process.
Frequently asked questions (FAQs)
How long does the prior authorization process typically take? On average, the approval process takes about 3-14 business days, though this can vary based on the specific service and insurance provider.
Can patients request their own prior authorization? In most cases, it is the responsibility of the provider to submit the CA Prior to Ordering Form, but patients can initiate the request by discussing their needs with their healthcare professional.
What happens if an urgent authorization is needed? If a request is deemed urgent, providers should indicate this clearly on the form, triggering an expedited review process that can yield results quickly.
What are the common reasons for denial? Denials often occur due to insufficient documentation, lack of medical necessity, or non-compliance with the insurer’s protocols.
Case studies
Success stories in streamlining the prior authorization process abound. For instance, a healthcare facility that implemented an electronic submission system saw a remarkable reduction in turnaround times. Their integration of pdfFiller allowed them to meet documentation requirements more efficiently, leading to quicker approvals and improved patient satisfaction.
Lessons learned from cases of denied and resubmitted applications reveal that completing each section meticulously, accompanied by robust clinical documentation, can significantly enhance approval rates. One facility noted that including clear rationale and patient history helped to overturn a denied authorization, allowing timely access to prescribed treatments.
Tools and resources for managing prior authorizations
pdfFiller offers a comprehensive suite of tools designed to enhance document management for prior authorizations. Users can highlight sections, add comments, and collaborate efficiently, making the submission process more straightforward. E-signature capabilities facilitate quick approvals from necessary parties without the delays associated with physical signatures.
In addition, other software applications can aid in tracking submissions, including task management apps that provide reminders for follow-ups and deadlines. Utilizing these digital solutions can help maintain organization and efficiency in handling multiple prior authorization requests simultaneously.






For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
How can I modify ca prior to ordering without leaving Google Drive?
How can I send ca prior to ordering to be eSigned by others?
How do I complete ca prior to ordering on an iOS device?
What is ca prior to ordering?
Who is required to file ca prior to ordering?
How to fill out ca prior to ordering?
What is the purpose of ca prior to ordering?
What information must be reported on ca prior to ordering?
pdfFiller is an end-to-end solution for managing, creating, and editing documents and forms in the cloud. Save time and hassle by preparing your tax forms online.