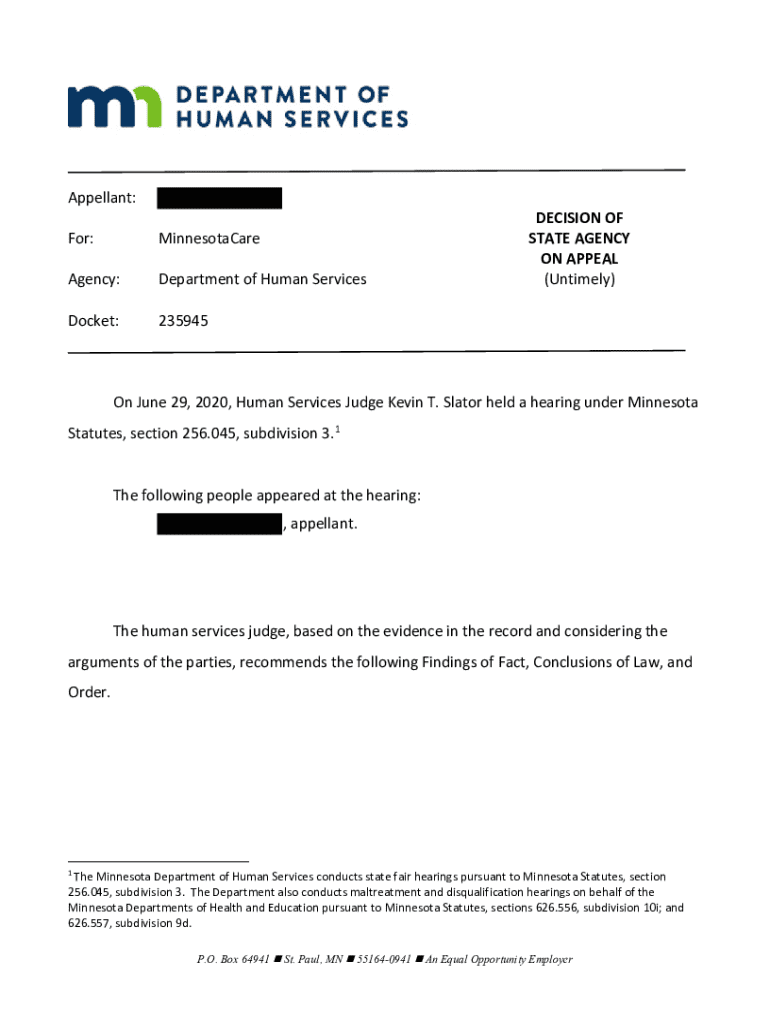
Get the free Appellant: For: MinnesotaCare Agency: Department of ... - MN.gov
Get, Create, Make and Sign appellant for minnesotacare agency



How to edit appellant for minnesotacare agency online
Uncompromising security for your PDF editing and eSignature needs
How to fill out appellant for minnesotacare agency

How to fill out appellant for minnesotacare agency
Who needs appellant for minnesotacare agency?
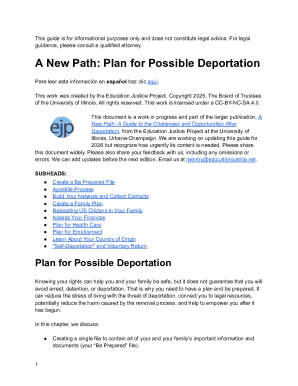
Appellant for Minnesotacare Agency Form: A Comprehensive Guide
Understanding the Minnesotacare program
Minnesotacare is a state-funded health care program designed to provide affordable health insurance for low- and moderate-income residents of Minnesota. The program aims to ensure that individuals without access to employer-sponsored insurance can receive necessary health services, emphasizing preventive care and basic medical needs.
Eligibility requirements for Minnesotacare include income limits, residency criteria, and age considerations. Generally, adults must have a household income at or below 200% of the federal poverty level, while children can qualify with different thresholds. Additionally, Minnesotacare serves adults, pregnant women, and children who do not qualify for Medical Assistance.
The benefits of Minnesotacare encompass a wide range of medical services, including doctor visits, hospital stays, preventive services, and mental health care. Accessing these services efficiently relies on the Minnesotacare agency form, crucial for enrollment and the overall claims process.
The Minnesotacare agency form plays a pivotal role in accessing health services. It's often required for significant actions like applying for benefits, making coverage changes, and appealing decisions regarding eligibility.
The appeals process: An overview
In the context of Minnesotacare, an appeal is a formal request for reconsideration regarding a decision made by the program—whether related to coverage, benefits, or other essential components of health care access. The appeals process is crucial for individuals contesting decisions they believe to be unfair or inaccurate.
Common reasons for filing an appeal include denied coverage for a particular service or treatment, incorrect benefits assigned to a policyholder, and unreasonable delays in processing claims. An effective appeal can assist in securing necessary medical care and ensuring that beneficiaries receive their entitled services.
Who can appeal?
Any individual who is a member of the Minnesotacare program has the right to file an appeal. This includes not only the primary insured person but also authorized representatives who may act on the beneficiary’s behalf, such as family members, guardians, or legal representatives.
Understanding who should fill out the Minnesotacare agency form is essential. If you are the primary policyholder, you are encouraged to submit the appeal yourself; however, if someone is acting on your behalf, they need to be designated as your representative formally in the appeal process.
Preparing to file your appeal
Before filing an appeal, it’s essential to gather all necessary documents. Start by collecting previous correspondence with Minnesotacare, including any denial letters, notices of coverage changes, and your current policy details. Medical records relevant to your case should also be compiled, particularly if they support the necessity of the service or treatment in question.
Another important aspect involves proving income and other eligibility documents. Pay stubs, tax returns, and proof of current household income will support your case if eligibility is questioned. Verify important timelines and deadlines; appealing should occur as soon as possible, typically within 30 days of receiving denied coverage notification.
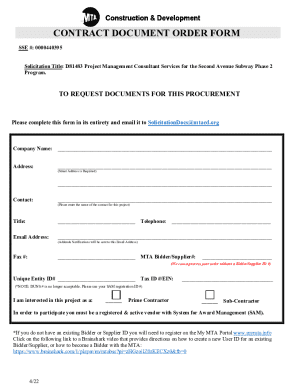
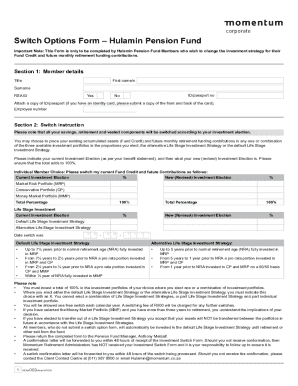
Step-by-step guide to completing the Minnesotacare agency form
Filling out the Minnesotacare agency form requires attention to detail. Start with your personal information, ensuring accuracy in your contact details and policy number. This will help streamline communication and expedite the review process.
Next, articulate the appeal description effectively. Clearly frame your case by concisely stating the specific issue and your reasoning for the appeal. Include any requests for particular outcomes or actions from Minnesotacare.
Ensure proper evidence submission. Attach relevant documents that substantiate your claims, such as medical records or financial documents. It’s vital to avoid common mistakes—such as incomplete information, missing or incorrect contact details, and insufficient evidence—that could delay or invalidate your appeal.
Submitting your appeal
Once your appeal is ready, consider your submission options. You can submit your appeal online through pdfFiller, ensuring a secure and efficient process. If you prefer, you can also mail your completed form or visit a local Minnesotacare office to submit it in person.
After submitting your appeal, you should receive confirmation from Minnesotacare regarding receipt of your documents. Understanding what to expect next helps in planning and reduces anxiety about the process.
After submission: What happens next?
Following the submission of your appeal, the review process begins. A designated team will assess your appeal based on the information provided. The review can take some time; often, individuals may experience delays before hearing back regarding the status. You can typically expect a decision within 30 to 45 days.
Potential outcomes include whether the appeal is granted, resulting in coverage of the contested services, or denied, which allows you to consider further options, including potential further appeals or informal hearings.
Do need a lawyer?
Seeking legal assistance can enhance your appeal strategy; however, it's not always necessary. Evaluating whether legal counsel is helpful depends on the complexity of your case. If your situation involves nuanced legal issues or if your first appeals are denied, hiring a legal representative might provide advantages.
A legal representative can assist in effectively framing the appeal, ensuring compliance with relevant regulations, and advocating aggressively for your rights in complicated cases. However, many successful appeals have been filed independently by motivated individuals.
What can appeal?
Understanding the specific decisions eligible for appeal can empower you during the process. Commonly appealed situations include denials of coverage for medical treatments, disagreements over the necessity of care, and disputes about eligibility for services.
Reviewing successful appeal cases can provide insight into crafting your appeal. Focus on personalizing your appeal to reflect the unique circumstances of your situation, which strengthens your argument for reconsideration.
Interactive tools and resources
Utilizing pdfFiller for document management enhances your appeal process. The platform allows seamless editing, signing, and collaboration on PDF forms, making managing all the required documentation straightforward.
Employing digital tools for tracking your appeal status simplifies the process. Regular updates on the status of your appeal can be vital for managing upcoming appointments or potential documentation requests.
Engaging with the Minnesota Department of Human Services (DHS)
Navigating the appeals process requires effective engagement with the Minnesota Department of Human Services (DHS). Understanding their role in facilitating appeals and providing support can enhance your experience.
To improve communication, prepare specific questions and documents for discussions with DHS representatives, as this proactive approach can clarify your individual case and expedite the necessary processes.






For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
How can I manage my appellant for minnesotacare agency directly from Gmail?
Can I sign the appellant for minnesotacare agency electronically in Chrome?
How do I fill out appellant for minnesotacare agency on an Android device?
What is appellant for minnesotacare agency?
Who is required to file appellant for minnesotacare agency?
How to fill out appellant for minnesotacare agency?
What is the purpose of appellant for minnesotacare agency?
What information must be reported on appellant for minnesotacare agency?
pdfFiller is an end-to-end solution for managing, creating, and editing documents and forms in the cloud. Save time and hassle by preparing your tax forms online.