Daily Nurses Notes - Page 2
What is Daily Nurses Notes?
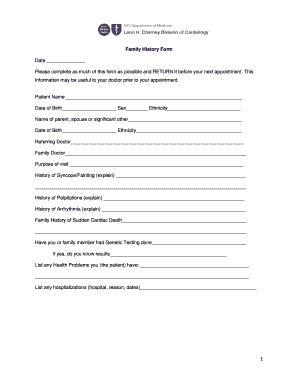
Daily Nurses Notes are detailed records kept by nurses to document the care given to patients on a daily basis. These notes are crucial in ensuring the continuity of care and providing important information for other healthcare providers.
What are the types of Daily Nurses Notes?
There are several types of Daily Nurses Notes based on the specific needs and requirements of the healthcare facility. Some common types include:
How to complete Daily Nurses Notes
Completing Daily Nurses Notes accurately and efficiently is essential for providing quality patient care. Here are some tips to help you complete Daily Nurses Notes effectively:
pdfFiller empowers users to create, edit, and share documents online. Offering unlimited fillable templates and powerful editing tools, pdfFiller is the only PDF editor users need to get their documents done.