What is Discharge Summary Format?
A discharge summary format is a structured document that provides a concise summary of a patient's hospital stay and the care they received. It contains essential information about the patient's medical history, diagnoses, procedures performed, medications prescribed, and recommendations for follow-up care. Discharge summary formats serve as an important communication tool between healthcare providers and ensure continuity of care for the patient.
What are the types of Discharge Summary Format?
There are several types of discharge summary formats that healthcare providers may use. The most common ones include:
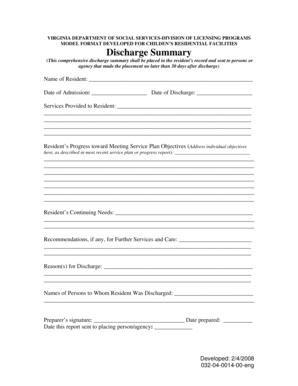
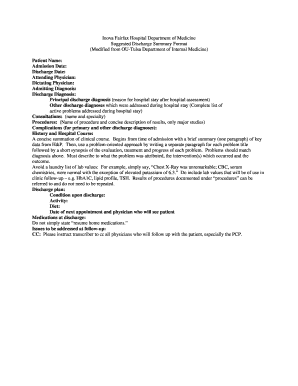
Traditional Discharge Summary Format: This format follows a standardized structure and includes sections such as patient demographics, diagnoses, treatment received, medications prescribed, and discharge instructions.
Modified Discharge Summary Format: Some healthcare facilities customize the traditional format to include additional sections or specific information based on their requirements.
Electronic Discharge Summary Format: With the advent of electronic health records (EHRs), many hospitals and clinics have transitioned to electronic discharge summary formats. These formats are generated and stored electronically, allowing for easier access, sharing, and updating of patient information.
How to complete Discharge Summary Format
Completing a discharge summary format requires attention to detail and accuracy. Here are the steps to follow:
01
Start with the patient's demographics: Include their name, age, gender, date of admission and discharge, and contact information.
02
Describe the reason for admission: Provide a brief summary of the patient's condition or symptoms that led to their hospitalization.
03
Outline the medical history: Include important information about the patient's past illnesses, surgeries, allergies, and chronic conditions.
04
Detail the treatment received: Describe the procedures, surgeries, medications, and therapies administered to the patient during their hospital stay.
05
Include discharge recommendations: Provide instructions for post-discharge care, follow-up appointments, medication instructions, and any dietary or activity restrictions.
06
Review and proofread: Ensure that the discharge summary format is accurate, complete, and free of any errors or inconsistencies before finalizing it.
pdfFiller empowers users to create, edit, and share documents online. Offering unlimited fillable templates and powerful editing tools, pdfFiller is the only PDF editor users need to get their documents done.