What is Discharge Summary?
A Discharge Summary is a document that provides a summary of a patient's stay in a healthcare facility, such as a hospital or clinic. It includes important information about the patient's diagnosis, treatment, and any medications prescribed. The Discharge Summary is typically prepared by the healthcare provider and is shared with the patient, as well as other healthcare professionals involved in the patient's care.
What are the types of Discharge Summary?
There are different types of Discharge Summaries, depending on the nature of the patient's condition and the level of care provided. Some common types include:
General Discharge Summary: Provides a general overview of the patient's stay, diagnosis, treatment, and recommendations for follow-up care.
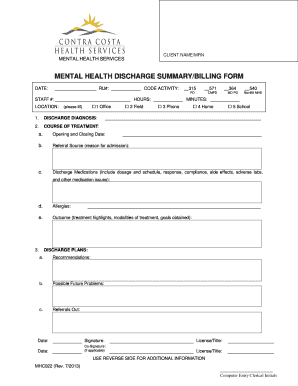
Psychiatric Discharge Summary: Focuses on the specific needs of patients with mental health conditions, discussing their treatment plan, medications, and recommendations for ongoing therapy or support.
Surgical Discharge Summary: Documents the details of a surgical procedure, including preoperative and postoperative care, any complications, and instructions for wound healing and recovery.
Maternity Discharge Summary: Pertains to patients who have given birth, covering topics such as the delivery process, postpartum care, and guidance for newborn care.
How to complete Discharge Summary
Completing a Discharge Summary involves several steps to ensure accurate and comprehensive documentation. Here is a step-by-step guide:
01
Gather necessary patient information, including their medical history, test results, and any consultations with other specialists.
02
Review the patient's progress during their stay and summarize their diagnosis, treatment plan, and response to therapy.
03
Include details about any medications prescribed, including dosage, frequency, and potential side effects.
04
Provide recommendations for follow-up care, such as scheduling appointments, ordering tests, or referring the patient to other healthcare professionals if necessary.
05
Proofread the Discharge Summary for errors or missing information and make any necessary revisions.
06
Share the completed Discharge Summary with the patient and other relevant healthcare professionals to ensure continuity of care.
pdfFiller empowers users to create, edit, and share documents online. Offering unlimited fillable templates and powerful editing tools, pdfFiller is the only PDF editor users need to get their documents done.