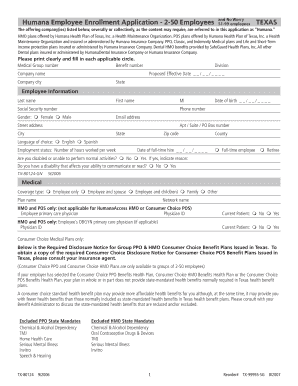
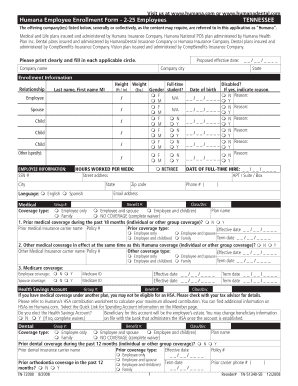
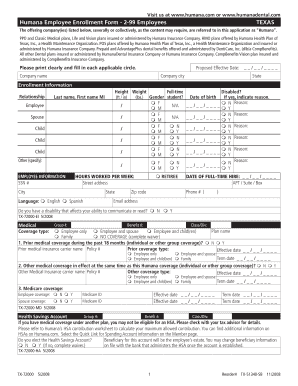
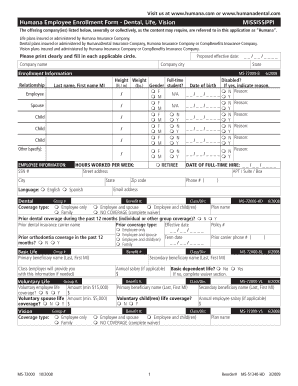
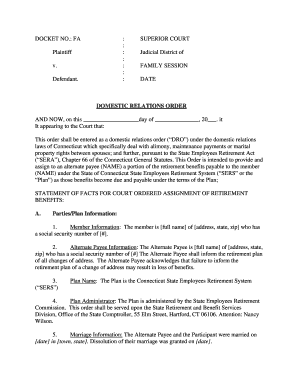
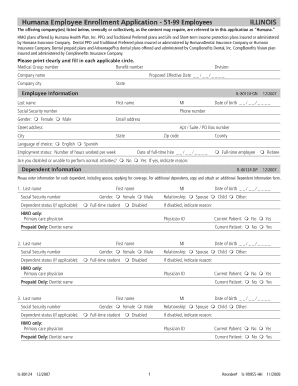
What is Humana Medical Claim Form?
Humana Medical Claim Form is a standardized document used by policyholders to request reimbursement for medical expenses incurred. This form is necessary to file a claim with Humana insurance and should be filled out accurately and in detail to ensure timely processing of the claim.
What are the types of Humana Medical Claim Form?
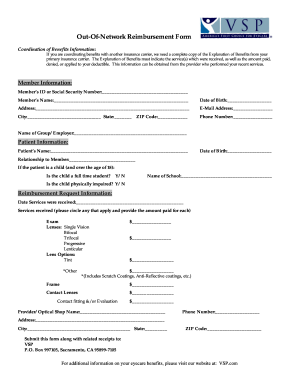
Humana offers different types of Medical Claim Forms depending on the specific insurance plan and the type of medical service or expense being claimed. The most commonly used forms include:
CMS-This form is used for submitting claims for professional services, such as doctor visits, laboratory tests, and outpatient procedures.
UB-This form is used for hospital-related services, including inpatient stays, surgeries, and specialized treatments.
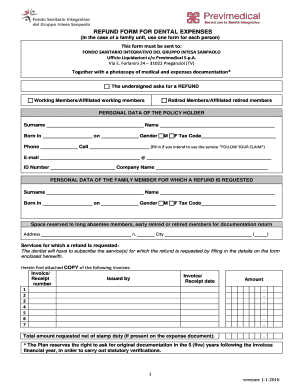
Dental Claim Form: This form is used for dental services and treatments.
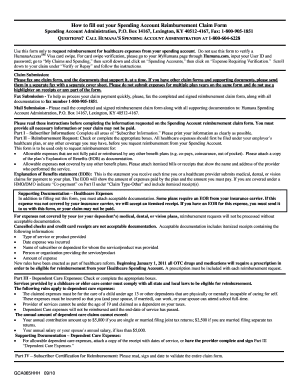
How to complete Humana Medical Claim Form?
Completing the Humana Medical Claim Form accurately is crucial to ensure prompt processing of the claim. Here are the steps to fill out the form:
01
Provide personal information: Start by providing your personal details, including name, address, date of birth, and contact information.
02
Include insurance details: Input your Humana insurance policy number, group number, and any other relevant insurance information.
03
Describe the medical service: Clearly explain the type of service or procedure being claimed, including the date it was performed.
04
Attach supporting documents: If there are any receipts, bills, or medical records related to the claim, make sure to attach them securely to the form.
05
Sign and submit: Review the completed form for accuracy and sign it. Submit the form along with any supporting documents to the designated Humana claim submission address.
pdfFiller empowers users to create, edit, and share documents online. Offering unlimited fillable templates and powerful editing tools, pdfFiller is the only PDF editor users need to get their documents done.