Example Of Prior Authorization Form - Page 2
What is an Example of a prior authorization form?
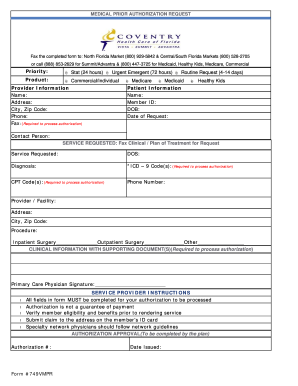
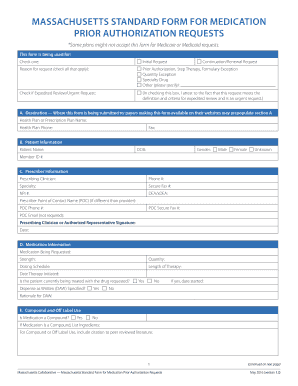
An Example of a prior authorization form is a document used by healthcare providers to request approval from insurance companies before providing certain services or medications to patients. This form helps ensure that the treatment is medically necessary and covered by the patient's insurance plan.
What are the types of Example of prior authorization form?
There are several types of prior authorization forms, including:
Medication prior authorization form
Medical procedure prior authorization form
Durable medical equipment prior authorization form
How to complete an Example of prior authorization form
Completing an Example of a prior authorization form is essential for a smooth approval process. Here are the steps to follow:
01
Fill in your personal information accurately
02
Provide details about the healthcare provider and the prescribed treatment or medication
03
Attach any necessary supporting documents, such as medical records or test results
04
Review the form for completeness and accuracy before submission
pdfFiller empowers users to create, edit, and share documents online, offering unlimited fillable templates and powerful editing tools. It is the only PDF editor users need to get their documents done efficiently.
Video Tutorial How to Fill Out Example of prior authorization form
Thousands of positive reviews can’t be wrong
Read more or give pdfFiller a try to experience the benefits for yourself
Questions & answers
What is a prior authorization when and why would one be needed?
Prior authorization—sometimes called precertification or prior approval—is a health plan cost-control process by which physicians and other health care providers must obtain advance approval from a health plan before a specific service is delivered to the patient to qualify for payment coverage.
What is a common example of when prior authorization may be required by a payer?
Ordering prescriptions outside of normal practice often results in the need to submit a prior authorization to the patient's plan. It can also be beneficial to create lists of medications and procedures that are covered by each plan.
What are the most common ways that prior authorization can be performed?
These steps are usually done manually, often through a cascade of phone calls, faxes and emails between payer and provider. The responsibility falls on the provider to continue to follow up with the insurance company until there is resolution of the prior authorization request — an approval, redirection, or denial.
What is an example of prior authorization?
For example, your health plan may require prior authorization for an MRI, so that they can make sure that a lower-cost x-ray wouldn't be sufficient. The service isn't being duplicated: This is a concern when multiple specialists are involved in your care.
What is a common class of medication that often requires a prior authorization?
Insurance companies will most likely require prior authorizations for the following drugs: Brand-name drugs that have a generic available. Drugs that are intended for certain age groups or conditions only. Drugs used only for cosmetic reasons.
How do I write a prior authorization letter for medication?
Dear <Medical Director Name and/or Medical Review/Appeals>: I am writing to request authorization for <Product Name> for my patient, <Patient Name>. I have prescribed <Product Name> because this patient has been diagnosed with <diagnosis>, and I believe that therapy with <Product Name> is appropriate for this patient.