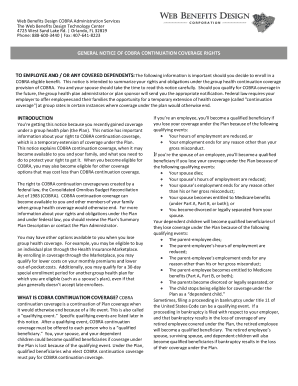
Cobra General Notice 2020
What is Cobra general notice 2020?
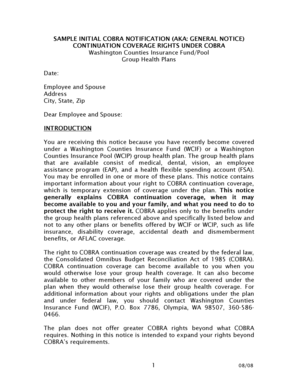
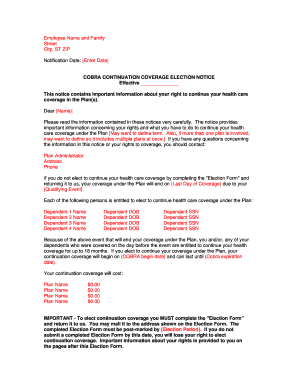
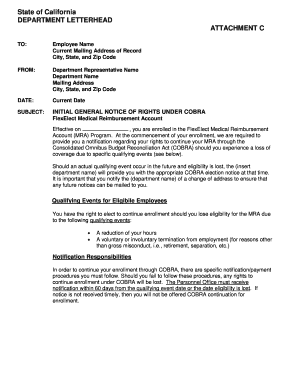
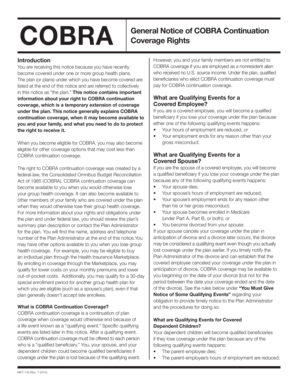
The Cobra general notice 2020 is a notification issued by the government that provides information on the rights and options available to employees and their families when it comes to continuing health insurance coverage after experiencing a qualifying event.
What are the types of Cobra general notice 2020?
There are typically two main types of Cobra general notice 2020 that employers are required to provide to their employees: the initial notice which must be sent within a certain timeframe after a qualifying event occurs, and the election notice which explains the individual's rights to elect continuation coverage.
How to complete Cobra general notice 2020
Completing the Cobra general notice 2020 is a straightforward process that involves following these steps:
pdfFiller empowers users to create, edit, and share documents online. Offering unlimited fillable templates and powerful editing tools, pdfFiller is the only PDF editor users need to get their documents done.