Cobra Letter To Employee 2020
What is Cobra letter to employee 2020?
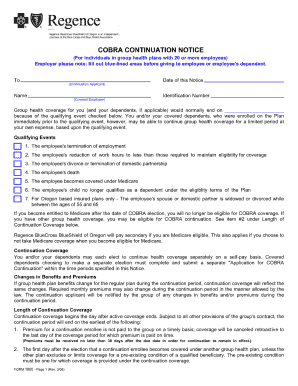
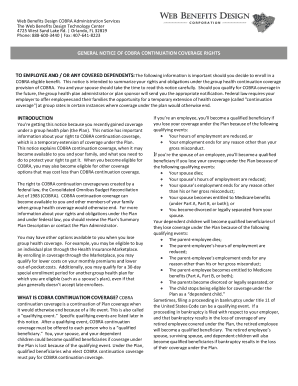
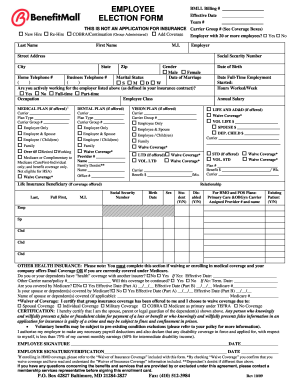
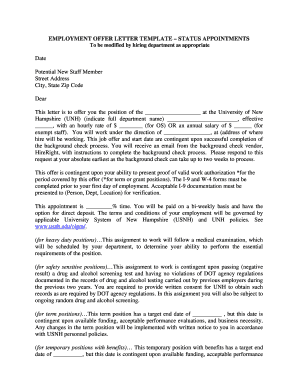
The Cobra letter to employee in 2020 is a notification that informs employees of their rights to continue their employer-sponsored health insurance coverage after experiencing a qualifying event that would otherwise result in loss of coverage.
What are the types of Cobra letter to employee 2020?
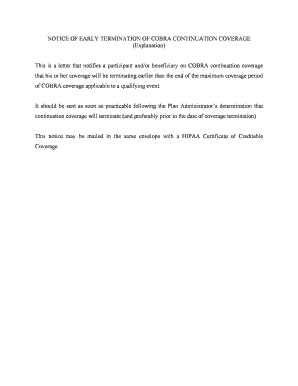
There are three main types of Cobra letters that employees may receive in 2020:
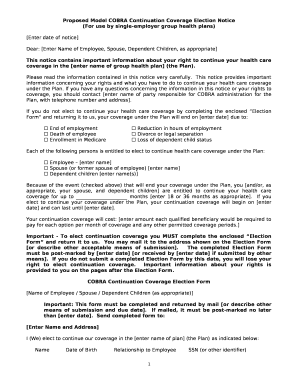
General notice: Sent to employees who are newly eligible for Cobra coverage.
Qualifying event notice: Sent to employees when a qualifying event occurs, triggering their right to elect Cobra coverage.
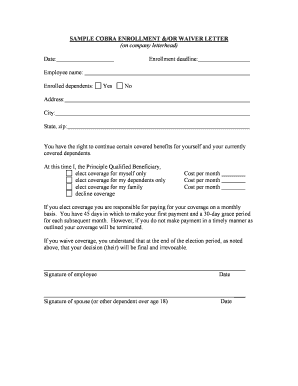
Decision notice: Sent to employees who have elected Cobra coverage, confirming their enrollment and providing payment information.
How to complete Cobra letter to employee 2020
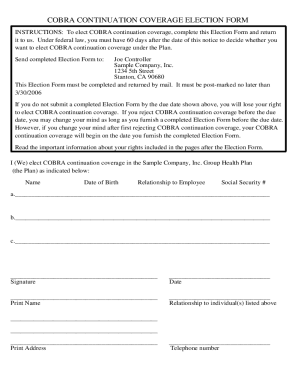
Completing the Cobra letter as an employee is a simple process that involves the following steps:
01
Read the letter carefully to understand your rights and options.
02
Fill out any required forms or election notices included with the letter.
03
Submit the completed forms to the designated party by the specified deadline.
pdfFiller empowers users to create, edit, and share documents online. Offering unlimited fillable templates and powerful editing tools, pdfFiller is the only PDF editor users need to get their documents done.
Video Tutorial How to Fill Out Cobra letter to employee 2020
Thousands of positive reviews can’t be wrong
Read more or give pdfFiller a try to experience the benefits for yourself
Questions & answers
Why would I receive a letter from COBRA?
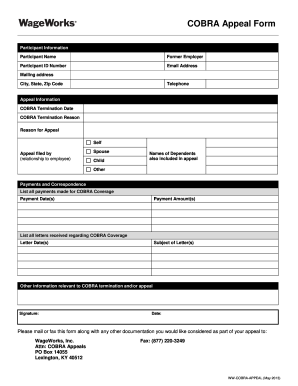
Qualifying Event: At the end of your employment or because of reduction of hours (not maintain full-time status) you will receive this letter. It is VERY important that you review this letter and make your decision if you will need to continue your coverage through COBRA.
What is the COBRA general notice?
COBRA General Notice Group health plans must give each employee and spouse a general notice describing COBRA rights within the first 90 days of coverage. Group health plans can satisfy this requirement by including the general notice in the plan's SPD and giving it to the employee and spouse within this time limit.
What triggers COBRA letter?
COBRA Qualifying Event Notice The employer must notify the plan if the qualifying event is: Termination or reduction in hours of employment of the covered employee, • Death of the covered employee, • Covered employee becoming entitled to Medicare, or • Employer bankruptcy.
When should COBRA general notice be sent?
The notice must be provided within the first 90 days of coverage under the group health plan. The general notice must include the following information: The name of the plan and the name, address and telephone number of someone the employee and spouse can contact for more information on COBRA and the plan.
What does it mean when you get a COBRA letter in the mail?
COBRA stands for the Consolidated Omnibus Budget Reconciliation Act. COBRA allows former employees, retirees, and their dependents to temporarily keep their health coverage. If you get COBRA, you must pay for the entire premium, including any portion that your employer may have paid in the past.
Do COBRA letters need to be sent certified?
Employers should send notices by first-class mail, obtain a certificate of mailing from the post office, and keep a log of letters sent. Certified mailing should be avoided, as a returned receipt with no delivery acceptance signature proves the participant did not receive the required notice.