Prior Authorization Form Pdf
What is Prior authorization form pdf?
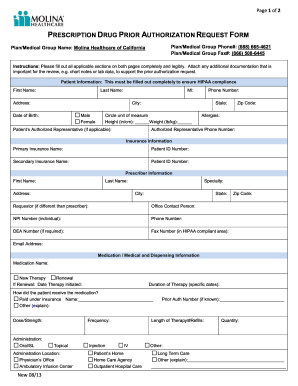
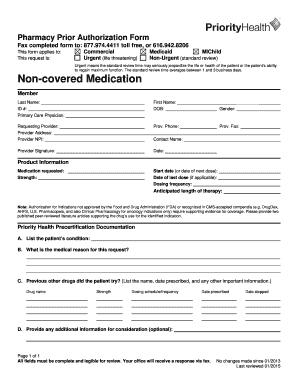
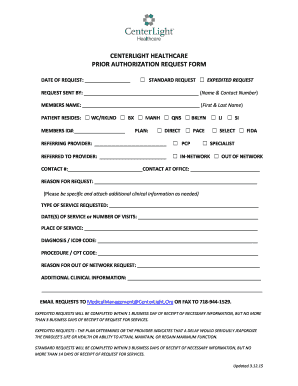
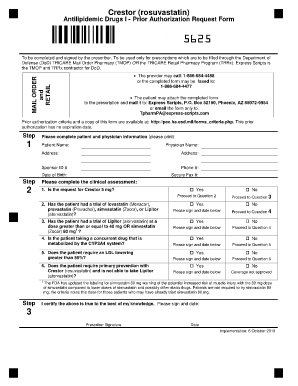
A Prior authorization form pdf is a document that healthcare providers need to submit to insurance companies to request coverage for certain medical services, treatments, or medications. This form is necessary to ensure that the insurance company will pay for the necessary services before the healthcare provider administers them.
What are the types of Prior authorization form pdf?
There are several types of Prior authorization form pdf, including:
Standard Prior Authorization Form
Urgent Prior Authorization Form
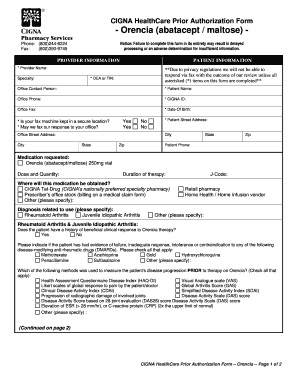
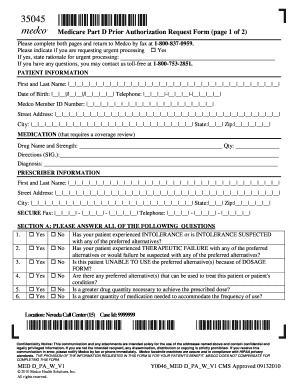
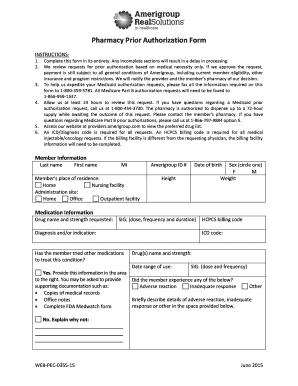
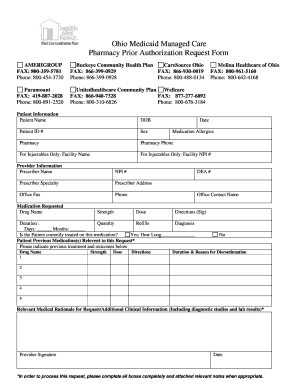
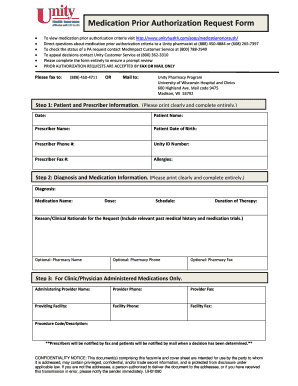
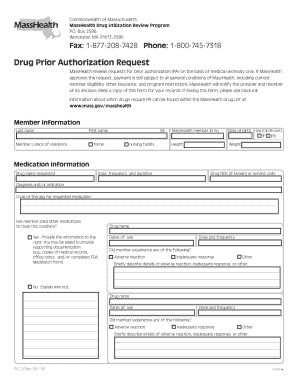
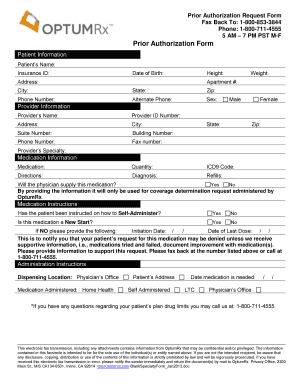
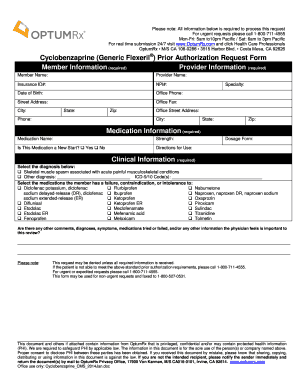
Medication Prior Authorization Form
Procedure Prior Authorization Form
How to complete Prior authorization form pdf
Completing a Prior authorization form pdf is a straightforward process. Here are the steps to follow:
01
Gather all necessary information related to the medical service, treatment, or medication being requested.
02
Fill out the patient's personal information accurately.
03
Provide details about the healthcare provider and the services being requested.
04
Include any supporting documentation or medical records that may be required.
05
Submit the completed form to the insurance company for review and approval.
pdfFiller empowers users to create, edit, and share documents online. Offering unlimited fillable templates and powerful editing tools, pdfFiller is the only PDF editor users need to get their documents done.
Video Tutorial How to Fill Out Prior authorization form pdf
Thousands of positive reviews can’t be wrong
Read more or give pdfFiller a try to experience the benefits for yourself
Questions & answers
Why do prior authorizations get denied?
Prior Authorization Denial Reasons Above all else, they want to make sure that you're providing the most cost-effective treatment. Other common reasons for preauthorization denials include: Misspelled names, incorrect billing codes, and other clerical errors.
How do I write a prior authorization?
Here is a sample prior authorization request form. Identifying information for the member/patient such as: Identifying information for the referring provider and servicing provider. Clinical information specific to the treatment requested that the payer can use to establish medical necessity, such as:
How long should I wait for a prior authorization?
How long does a prior authorization take? Depending on the complexity of the prior authorization request, the level of manual work involved, and the requirements stipulated by the payer, a prior authorization can take anywhere from one day to a month to process.
Is prior authorization difficult?
The process involve in the prior authorization is sometimes complex and complicated as it sometimes may require the input of even more than one insurer (4).
How do I get prior authorization for medication?
Prior authorization works like this: Step 1: If your doctor didn't contact your insurance company when prescribing a medication, your pharmacy will contact them. Step 2: The physician (or their staff) will contact the insurance company. Step 3: Your insurance provider may want you to fill out and sign some forms.
Why is it so hard to get a prior authorization?
Insurance companies can deny a request for prior authorization for reasons such as: The doctor or pharmacist didn't complete the necessary steps. Filling the wrong paperwork or missing information such as service code or date of birth.