Replace Brand Logo in Soap Note
Drop document here to upload
Up to 100 MB for PDF and up to 25 MB for DOC, DOCX, RTF, PPT, PPTX, JPEG, PNG, JFIF, XLS, XLSX or TXT
Note: Integration described on this webpage may temporarily not be available.
0
Forms filled
0
Forms signed
0
Forms sent
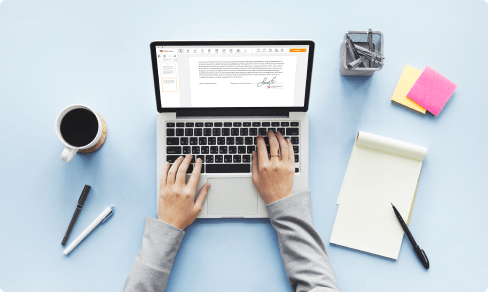
Upload your document to the PDF editor
Type anywhere or sign your form

Print, email, fax, or export

Try it right now! Edit pdf
Introducing Soap Note Replace Brand Logo Feature
Are you looking to add a personal touch to your SOAP notes? Look no further! Our Soap Note Replace Brand Logo feature is here to impress.
Key Features:
Customize SOAP notes with your brand's logo
Easy to use interface for quick editing
Seamless integration with existing templates
Potential Use Cases and Benefits:
Enhance professionalism and branding in your medical practice
Build trust with patients by showcasing a recognizable logo
Save time by quickly personalizing notes for each patient
Say goodbye to generic SOAP notes and hello to a personalized touch with our Soap Note Replace Brand Logo feature. Elevate your practice and make a lasting impression on your patients!
All-in-one PDF software
A single pill for all your PDF headaches. Edit, fill out, eSign, and share – on any device.
How to Replace Brand Logo in Soap Note
01
Enter the pdfFiller website. Login or create your account for free.
02
Using a protected internet solution, you are able to Functionality faster than ever.
03
Enter the Mybox on the left sidebar to access the list of your documents.
04
Select the template from the list or click Add New to upload the Document Type from your desktop or mobile device.
Alternatively, you are able to quickly transfer the desired template from well-known cloud storages: Google Drive, Dropbox, OneDrive or Box.
Alternatively, you are able to quickly transfer the desired template from well-known cloud storages: Google Drive, Dropbox, OneDrive or Box.
05
Your document will open inside the feature-rich PDF Editor where you could change the template, fill it out and sign online.
06
The powerful toolkit allows you to type text on the form, put and modify photos, annotate, and so forth.
07
Use sophisticated functions to incorporate fillable fields, rearrange pages, date and sign the printable PDF document electronically.
08
Click on the DONE button to finish the adjustments.
09
Download the newly created document, distribute, print out, notarize and a lot more.
What our customers say about pdfFiller
See for yourself by reading reviews on the most popular resources:
Dustin Smallheer
2018-12-20

Annette Duplechin
2019-01-29
What do you like best?
Easy accessibility, signature verification, conversion to other formats, storage of documents, and ability to share to multiple platforms.
What do you dislike?
Zip Files - have to open and resave docs needed for uploading to other sources.
Recommendations to others considering the product:
Must be familiar with Zip files; Dashboard is super user-friendly; would not recommend for an occasional user - should have consistent need for the various services it provides.
What problems are you solving with the product? What benefits have you realized?
A quick and easy tool for conversion of docs to other formats compatible for social media marketing. And easy signature option of docs required for business transactions.
Easy accessibility, signature verification, conversion to other formats, storage of documents, and ability to share to multiple platforms.
What do you dislike?
Zip Files - have to open and resave docs needed for uploading to other sources.
Recommendations to others considering the product:
Must be familiar with Zip files; Dashboard is super user-friendly; would not recommend for an occasional user - should have consistent need for the various services it provides.
What problems are you solving with the product? What benefits have you realized?
A quick and easy tool for conversion of docs to other formats compatible for social media marketing. And easy signature option of docs required for business transactions.

For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
What if I have more questions?
Contact Support
What does SOAP notes stand for?
The SOAP note (an acronym for subjective, objective, assessment, and plan) is a method of documentation employed by health care providers to write out notes in a patient's chart, along with other common formats, such as the admission note.
What is the A in SOAP notes?
A SOAP note is information about the patient, which is written or presented in a specific order, which includes certain components. ... If everyone used a different format, it can get confusing when reviewing a patient's chart. A SOAP note consists of four sections including subjective, objective, assessment and plan.
What does the A stand for in SOAP notes?
The SOAP note (an acronym for subjective, objective, assessment, and plan) is a method of documentation employed by health care providers to write out notes in a patient's chart, along with other common formats, such as the admission note.
What is soap in physical therapy?
SOAP stands for Subjective, Objective, Assessment and Plan. If you want to write Physical Therapist SOAP notes that help you, your patient and their whole care team, include these elements outlined by the American Physical Therapy Association: Self-report of the patient. Details of the specific intervention provided.
How do you write a SOAP note?
0:45
6:33
Suggested clip
SOAP NOTES - YouTubeYouTubeStart of suggested clipEnd of suggested clip
SOAP NOTES - YouTube
What does SOAP notes stand for massage?
Massage therapists and other health care professionals often use SOAP notes to document clients' health records. SOAP notes (an acronym for subjective, objective, assessment, and plan) have become a standardized form of note-taking and are critically important for a variety reasons.
What does SOAP stand for in massage?
SOAP (an acronym for Subjective, Objective, Assessment, and Plan) is a method of documentation employed by health care providers including massage therapists to write out notes in a patient's chart.
What do SOAP notes stand for?
The SOAP note (an acronym for subjective, objective, assessment, and plan) is a method of documentation employed by health care providers to write out notes in a patient's chart, along with other common formats, such as the admission note.
Are massage therapists required to keep SOAP notes?
The answer is actually YES, you do! YES You do need to maintain current client files. YES You must have consent forms and HIPPA forms. YES You need to maintain notes of all sessions.
Why do we use SOAP notes?
SOAP notes. Today, the SOAP note an acronym for Subjective, Objective, Assessment and Plan is the most common method of documentation used by providers to input notes into patients' medical records. They allow providers to record and share information in a universal, systematic and easy to read format.
Other ready to use document templates
eSignature workflows made easy
Sign, send for signature, and track documents in real-time with signNow.




I have been using PDFiller for 2 years now, and it doesn't disappoint! It is easy to navigate around, and just as easy to save on to your computer, send as email or just print right away. I also like the new function of saving repeated work as a template. Thanks so much for a great product!
What do you dislike?
There's nothing that I would say is wrong with this program! I have never had an issue!!
Recommendations to others considering the product:
Use it! Super simple to naviagte!!
What problems are you solving with the product? What benefits have you realized?
I am able to work quickly on documents that I need for my foodservice operation. PDFiller makes it easy to taper any document to my specific customers needs.