Humana Out Of Network Claim Form
What is humana out of network claim form?
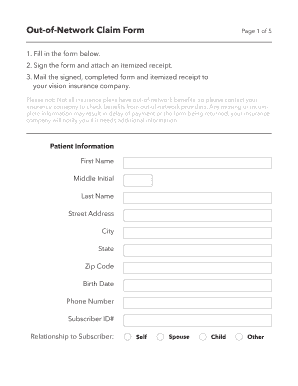
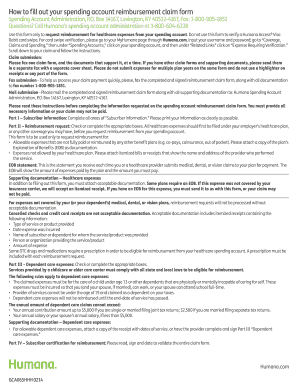
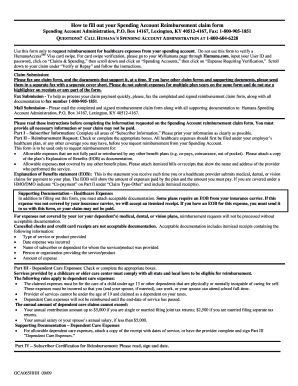
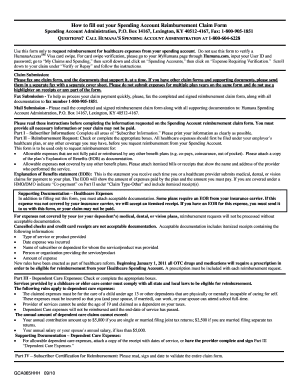
The humana out of network claim form is a document that needs to be filled out in order to request reimbursement for medical services received from healthcare providers that do not participate in the humana network. This form allows humana members to submit claims for out-of-network services and be reimbursed for eligible expenses.
What are the types of humana out of network claim form?
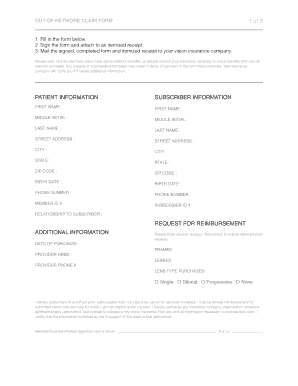
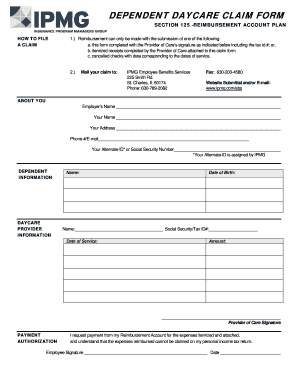
There are several types of humana out of network claim forms, depending on the type of medical service received. Some common types include: 1. Medical Claim Form: Used to request reimbursement for medical services such as doctor visits, surgeries, or hospital stays. 2. Prescription Drug Claim Form: Used to request reimbursement for prescription medications purchased outside of the humana network. 3. Dental Claim Form: Used to request reimbursement for dental services received from out-of-network providers. 4. Vision Claim Form: Used to request reimbursement for vision-related expenses, such as eye exams or glasses, when provided by out-of-network providers.
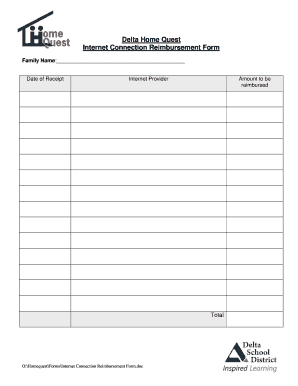
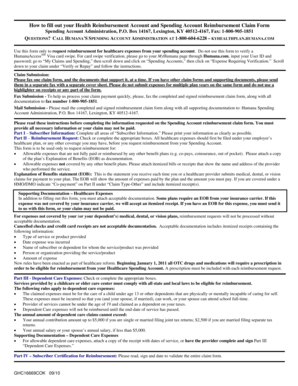
How to complete humana out of network claim form
To complete a humana out of network claim form, follow these simple steps: 1. Obtain the correct claim form: Determine the type of medical service received and select the corresponding claim form from humana's official website or contact customer service for assistance. 2. Gather necessary documentation: Collect all relevant documents, including receipts, invoices, and any other supporting documentation. 3. Fill out the form: Carefully complete all sections of the claim form, providing accurate and detailed information. 4. Attach supporting documentation: Ensure all required documents are securely attached to the claim form. 5. Review and double-check: Before submitting, review the completed form and attached documents to make sure everything is accurate and complete. 6. Submit the claim: Send the completed claim form and supporting documentation to the designated address provided by humana. pdfFiller empowers users to create, edit, and share documents online. Offering unlimited fillable templates and powerful editing tools, pdfFiller is the only PDF editor users need to get their documents done.