Humana Provider Forms
What is humana provider forms?
Humana provider forms are documents that healthcare providers use to submit claims for reimbursement and to update their information with Humana, a leading healthcare company. These forms allow providers to efficiently communicate with Humana and ensure that they receive timely payments for the services they provide.
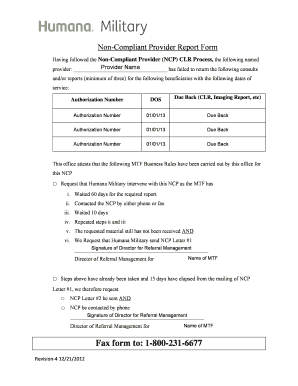
What are the types of humana provider forms?
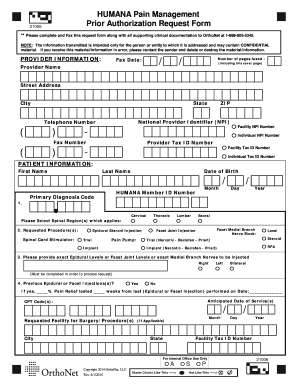
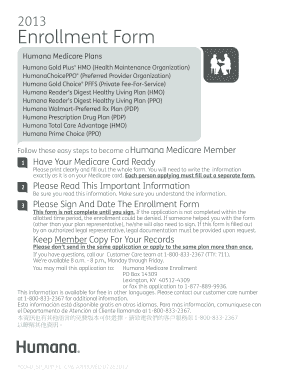
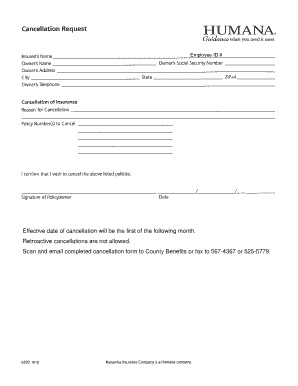
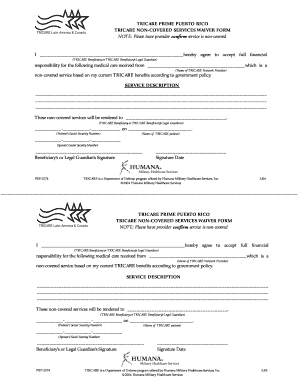
There are several types of humana provider forms that cater to different needs of healthcare providers. These forms include: 1. Claim Reimbursement Form: This form is used to request payment for healthcare services provided to patients. 2. Provider Information Update Form: Healthcare providers use this form to update their contact information, billing information, and any other relevant details. 3. Authorization Request Form: This form is used to request authorization from Humana for certain medical procedures or treatments. 4. Prior Authorization Form: Healthcare providers need to complete this form to obtain pre-approval for specific treatment or medications.
How to complete humana provider forms
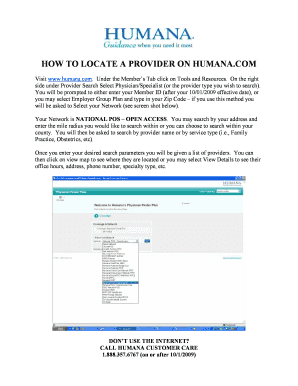
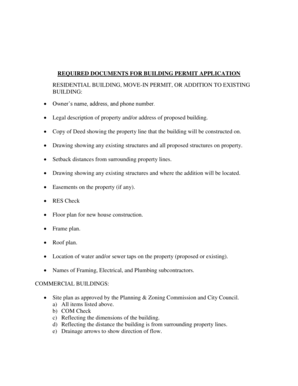
Completing humana provider forms accurately and thoroughly is essential to ensure timely processing and payment. Here is a step-by-step guide to help you complete these forms: 1. Obtain the form: Access the humana provider forms either through Humana's website or by contacting their customer service. 2. Read the instructions: Carefully review the instructions provided with the form to understand the requirements and any specific documentation needed. 3. Gather information: Collect all the necessary information and supporting documentation required to complete the form accurately. 4. Fill out the form: Enter the requested information in the appropriate fields, ensuring accuracy and completeness. 5. Double-check: Review the filled form for any errors or missing information. 6. Submit the form: Follow the submission instructions provided on the form or through Humana's submission process. 7. Keep copies: Make sure to keep copies of the completed forms and any supporting documentation for your records.
pdfFiller empowers users to create, edit, and share documents online. Offering unlimited fillable templates and powerful editing tools, pdfFiller is the only PDF editor users need to get their documents done.