Get the free Adjudication on Appeal for Reimbursement Denial - services dpw state pa
Show details
This document serves as the formal adjudication and recommendation on the appeal by UPMC Horizon Hospital against a denial of reimbursement for patient admission due to lack of medical necessity.
We are not affiliated with any brand or entity on this form
Get, Create, Make and Sign adjudication on appeal for
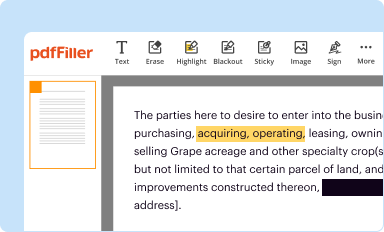
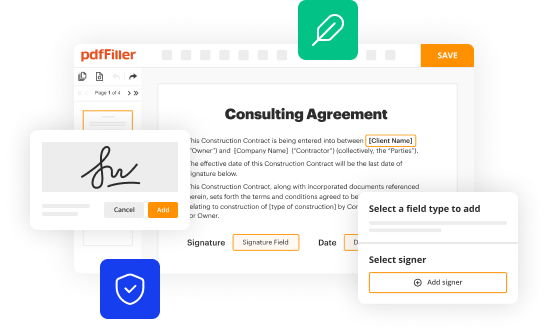
Edit your adjudication on appeal for form online
Type text, complete fillable fields, insert images, highlight or blackout data for discretion, add comments, and more.
Add your legally-binding signature
Draw or type your signature, upload a signature image, or capture it with your digital camera.
Share your form instantly
Email, fax, or share your adjudication on appeal for form via URL. You can also download, print, or export forms to your preferred cloud storage service.
How to edit adjudication on appeal for online
Here are the steps you need to follow to get started with our professional PDF editor:
1
Create an account. Begin by choosing Start Free Trial and, if you are a new user, establish a profile.
2
Prepare a file. Use the Add New button. Then upload your file to the system from your device, importing it from internal mail, the cloud, or by adding its URL.
3
Edit adjudication on appeal for. Rearrange and rotate pages, insert new and alter existing texts, add new objects, and take advantage of other helpful tools. Click Done to apply changes and return to your Dashboard. Go to the Documents tab to access merging, splitting, locking, or unlocking functions.
4
Get your file. When you find your file in the docs list, click on its name and choose how you want to save it. To get the PDF, you can save it, send an email with it, or move it to the cloud.
It's easier to work with documents with pdfFiller than you could have ever thought. Sign up for a free account to view.
Uncompromising security for your PDF editing and eSignature needs
Your private information is safe with pdfFiller. We employ end-to-end encryption, secure cloud storage, and advanced access control to protect your documents and maintain regulatory compliance.
How to fill out adjudication on appeal for
How to fill out Adjudication on Appeal for Reimbursement Denial
01
Gather all relevant documentation related to the reimbursement denial.
02
Review the denial letter to understand the reasons for the denial.
03
Complete the Adjudication on Appeal form, ensuring all fields are filled out accurately.
04
Clearly state your case, addressing the reasons for denial and providing evidence to support your claim.
05
Attach any supporting documents, such as receipts, medical records, or previous correspondence.
06
Double-check the form for completeness and accuracy before submission.
07
Submit the form and documentation to the appropriate appeals office by the specified deadline.
Who needs Adjudication on Appeal for Reimbursement Denial?
01
Individuals or patients who have had a reimbursement claim denied by an insurance company.
02
Healthcare providers seeking to appeal a denial on behalf of a patient.
03
Organizations or advocates assisting clients with reimbursement appeals.
Fill
form
: Try Risk Free






People Also Ask about
What does it mean when a claim has been adjudicated?
What is claims adjudication? Claims adjudication is the process by which insurance companies thoroughly review healthcare claims before reimbursement or payout. During this process, they decide whether to pay the claim in full, pay a partial amount, or deny it altogether.
Does adjudicated mean charged?
This process determines the outcome of a legal matter by analyzing evidence and applying relevant laws. Essentially, adjudication is the judicial decision-making that concludes whether a defendant is guilty or not guilty.
What does it mean when a payment is adjudicated?
Payment adjudication is the process in which agencies: • receive and review payment matches during Payment. Integration (i.e., at the time of payment), • verify the payment matches to determine whether they. are proper or improper, • record the results in the Do Not Pay (DNP) Portal.
What is an adjudicated payment?
Payment adjudication is the process in which agencies: • receive and review payment matches during Payment. Integration (i.e., at the time of payment), • verify the payment matches to determine whether they. are proper or improper, • record the results in the Do Not Pay (DNP) Portal.
What happens when a claim is adjudicated?
What is claims adjudication? Claims adjudication is a long and complex process that is used by a payor to evaluate a medical claim. They use it to determine how much will be reimbursed to a healthcare provider for administering care services.
Does adjudicated mean approved?
Adjudicate, which is usually used to mean "to make an official decision about who is right in a dispute," is one of several terms that give testimony to the influence of jus, the Latin word for "law," on our legal language.
What does adjudication mean in denials?
Adjudication refers to the overall process of reviewing and determining the payment or denial of a claim, while denial management specifically deals with the handling and resolution of denied claims.
What is an adjudication appeal?
Adjudication is a formal legal ruling issued by a court or tribunal, while arbitration is a private dispute resolution method that allows parties to choose their decision-maker and process. Arbitration is generally faster and more flexible, but adjudication provides stronger legal enforcement and broader appeal rights.
For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
What is Adjudication on Appeal for Reimbursement Denial?
Adjudication on Appeal for Reimbursement Denial is the process through which individuals or entities can challenge and request a review of a denial of reimbursement for expenses incurred, typically in healthcare or insurance contexts.
Who is required to file Adjudication on Appeal for Reimbursement Denial?
Generally, the party who received the initial reimbursement denial—such as patients, healthcare providers, or insurance policyholders—is required to file for Adjudication on Appeal for Reimbursement Denial.
How to fill out Adjudication on Appeal for Reimbursement Denial?
To fill out the Adjudication on Appeal for Reimbursement Denial, gather all relevant documentation including the original denial notice, billing statements, and any supporting evidence. Complete the form with clear details about the denial, reasons for contesting it, and any necessary personal or claimant information.
What is the purpose of Adjudication on Appeal for Reimbursement Denial?
The purpose of Adjudication on Appeal for Reimbursement Denial is to provide a mechanism for disputing a denial of reimbursement, allowing the claimant to present their case and potentially reverse the denial based on additional information or mitigated circumstances.
What information must be reported on Adjudication on Appeal for Reimbursement Denial?
Information that must be reported typically includes the claimant's details, insurance policy information, a description of the services or items denied, the reason for denial, and any evidence or documentation supporting the appeal.
Fill out your adjudication on appeal for online with pdfFiller!
pdfFiller is an end-to-end solution for managing, creating, and editing documents and forms in the cloud. Save time and hassle by preparing your tax forms online.

Adjudication On Appeal For is not the form you're looking for?Search for another form here.
Relevant keywords
Related Forms
If you believe that this page should be taken down, please follow our DMCA take down process
here
.
This form may include fields for payment information. Data entered in these fields is not covered by PCI DSS compliance.