
Get the free Consolidated Omnibus Reconciliation Act (COBRA) Update - calstate
Show details
This document provides details and updates on COBRA regulations affecting the California State University health plans, including eligibility, coverage periods, notices, and administrative procedures
We are not affiliated with any brand or entity on this form
Get, Create, Make and Sign consolidated omnibus reconciliation act
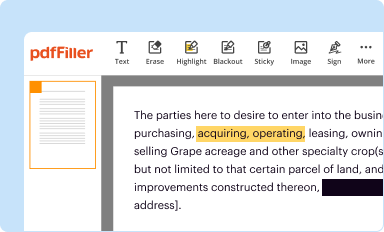
Edit your consolidated omnibus reconciliation act form online
Type text, complete fillable fields, insert images, highlight or blackout data for discretion, add comments, and more.
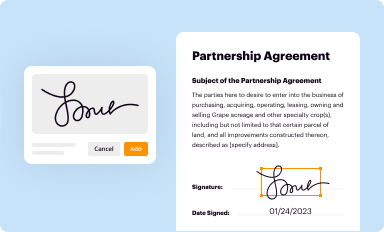
Add your legally-binding signature
Draw or type your signature, upload a signature image, or capture it with your digital camera.
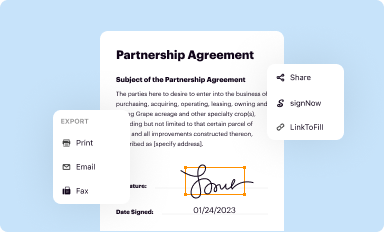
Share your form instantly
Email, fax, or share your consolidated omnibus reconciliation act form via URL. You can also download, print, or export forms to your preferred cloud storage service.
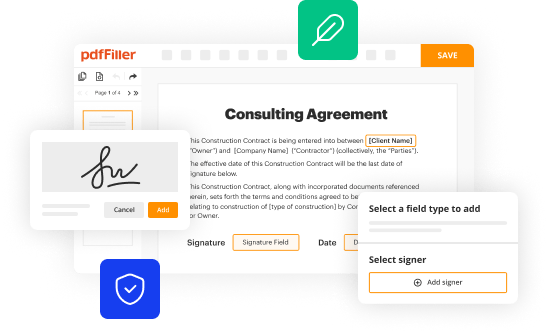
How to edit consolidated omnibus reconciliation act online
To use the services of a skilled PDF editor, follow these steps:
1
Create an account. Begin by choosing Start Free Trial and, if you are a new user, establish a profile.
2
Upload a document. Select Add New on your Dashboard and transfer a file into the system in one of the following ways: by uploading it from your device or importing from the cloud, web, or internal mail. Then, click Start editing.
3
Edit consolidated omnibus reconciliation act. Rearrange and rotate pages, insert new and alter existing texts, add new objects, and take advantage of other helpful tools. Click Done to apply changes and return to your Dashboard. Go to the Documents tab to access merging, splitting, locking, or unlocking functions.
4
Save your file. Select it in the list of your records. Then, move the cursor to the right toolbar and choose one of the available exporting methods: save it in multiple formats, download it as a PDF, send it by email, or store it in the cloud.
It's easier to work with documents with pdfFiller than you could have ever thought. You can sign up for an account to see for yourself.
Uncompromising security for your PDF editing and eSignature needs
Your private information is safe with pdfFiller. We employ end-to-end encryption, secure cloud storage, and advanced access control to protect your documents and maintain regulatory compliance.
How to fill out consolidated omnibus reconciliation act
How to fill out Consolidated Omnibus Reconciliation Act (COBRA) Update
01
Locate the COBRA Update form provided by your employer or health insurance administrator.
02
Read the instructions carefully to understand the information required.
03
Fill in your personal information, including name, address, and contact details.
04
Indicate the reason for the COBRA update, such as a change in address or beneficiary.
05
Provide information about your current health coverage under COBRA.
06
Review all entries to ensure accuracy and completeness.
07
Sign and date the form where required.
08
Submit the completed COBRA Update form to your employer or designated COBRA administrator.
Who needs Consolidated Omnibus Reconciliation Act (COBRA) Update?
01
Any employee who has recently experienced a qualifying event such as job loss, reduction in hours, or change in employment status.
02
Dependents of employees who qualify for COBRA benefits.
03
Individuals who wish to continue their health insurance coverage after leaving their job.
Fill
form
: Try Risk Free






People Also Ask about
What did the COBRA Act do?
COBRA stands for the Consolidated Omnibus Budget Reconciliation Act. COBRA allows former employees, retirees, and their dependents to temporarily keep their health coverage. If you get COBRA, you must pay for the entire premium, including any portion that your employer may have paid in the past.
What does the Consolidated Omnibus Budget Reconciliation Act (Cobra) do?
The Consolidated Omnibus Budget Reconciliation Act (COBRA) gives workers and their families who lose their health benefits the right to choose to continue group health benefits provided by their group health plan for limited periods of time under certain circumstances such as voluntary or involuntary job loss,
What did the Consolidated Omnibus Budget Reconciliation Act COBRA accomplish?
The Consolidated Omnibus Budget Reconciliation Act (COBRA) gives workers and their families who lose their health benefits the right to choose to continue group health benefits provided by their group health plan for limited periods of time under certain circumstances such as voluntary or involuntary job loss,
What does the Consolidated Omnibus Budget Reconciliation Act COBRA?
COBRA, the Consolidated Omnibus Budget Reconciliation Act, lets qualified workers keep their group health insurance for a limited time after a change in eligibility.
What is the 60 day COBRA loophole?
You have 60 days to enroll in COBRA once your employer-sponsored benefits end. Even if your enrollment is delayed, you will be covered by COBRA starting the day your prior coverage ended.
Is COBRA 18 months or 36 months?
In that case, COBRA lasts for eighteen months. If the qualifying event is the death of the covered employee, divorce or legal separation of the covered employee from the covered employee's spouse, or the covered employee becoming entitled to Medicare, COBRA for the spouse or dependent child lasts for 36 months.
For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
What is Consolidated Omnibus Reconciliation Act (COBRA) Update?
The Consolidated Omnibus Reconciliation Act (COBRA) Update refers to the periodic modifications and guidance related to the COBRA law, which allows employees and their dependents to continue health insurance coverage after employment ends or certain qualifying events occur.
Who is required to file Consolidated Omnibus Reconciliation Act (COBRA) Update?
Employers with group health plans, including private-sector employers with 20 or more employees, must file a COBRA Update to ensure compliance with the Act's regulations.
How to fill out Consolidated Omnibus Reconciliation Act (COBRA) Update?
To fill out a COBRA Update, employers must gather necessary data related to covered employees and qualifying events, complete the required forms, and submit them to the appropriate agency while ensuring all information is accurate and up to date.
What is the purpose of Consolidated Omnibus Reconciliation Act (COBRA) Update?
The purpose of the COBRA Update is to provide continued health insurance coverage to employees and their families after certain events, ensuring they do not lose access to healthcare due to job loss or other qualifying circumstances.
What information must be reported on Consolidated Omnibus Reconciliation Act (COBRA) Update?
Information required for the COBRA Update includes details about the group health plan, the qualifying events leading to coverage loss, eligible beneficiaries, and the duration of the COBRA coverage being offered.
Fill out your consolidated omnibus reconciliation act online with pdfFiller!
pdfFiller is an end-to-end solution for managing, creating, and editing documents and forms in the cloud. Save time and hassle by preparing your tax forms online.

Consolidated Omnibus Reconciliation Act is not the form you're looking for?Search for another form here.
Relevant keywords
Related Forms
If you believe that this page should be taken down, please follow our DMCA take down process
here
.
This form may include fields for payment information. Data entered in these fields is not covered by PCI DSS compliance.





















