Get the free 276/277 HEALTH CARE CLAIM STATUS REQUEST AND RESPONSE
Show details
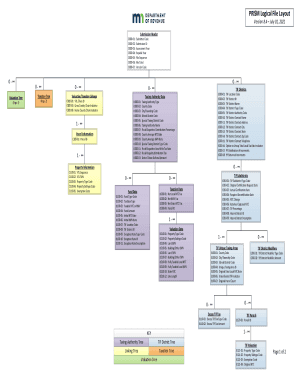
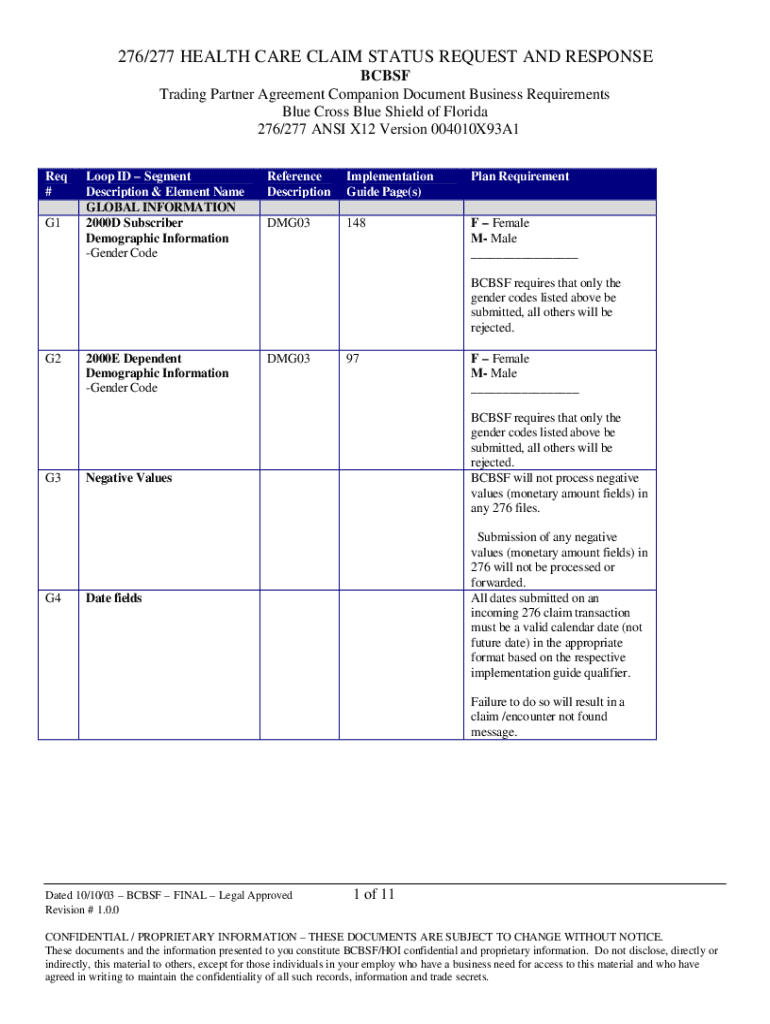
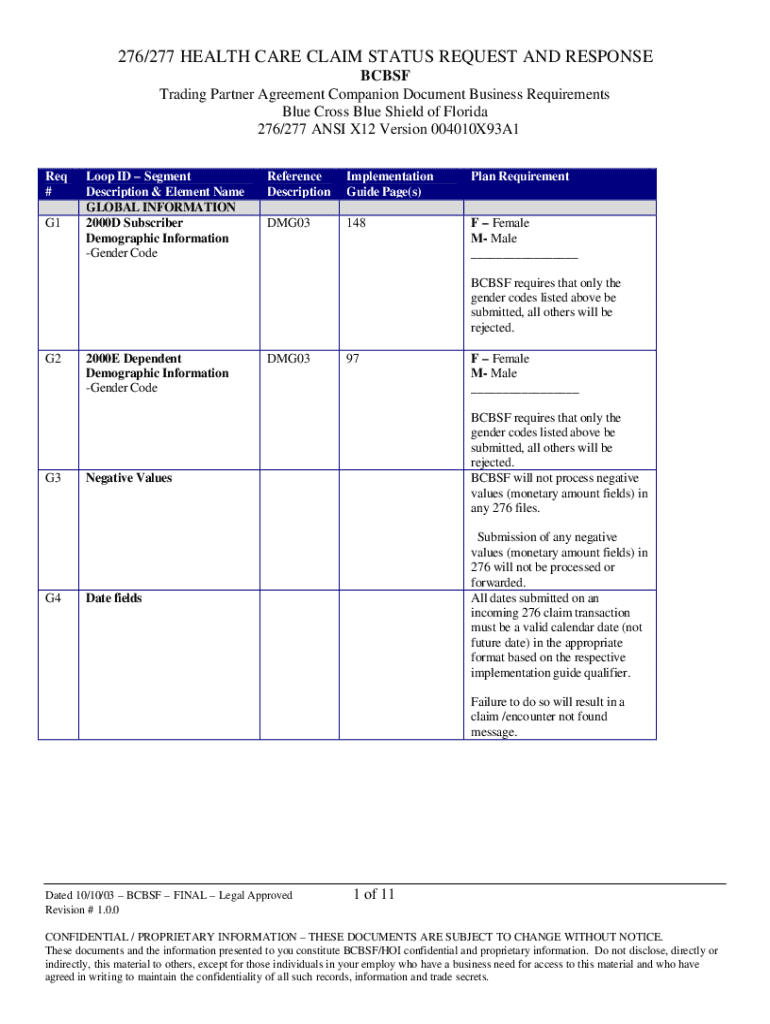
This document provides the business requirements and implementation guidelines for the 276/277 health care claim status request and response for Blue Cross Blue Shield of Florida.
We are not affiliated with any brand or entity on this form
Get, Create, Make and Sign 276277 health care claim

Edit your 276277 health care claim form online
Type text, complete fillable fields, insert images, highlight or blackout data for discretion, add comments, and more.

Add your legally-binding signature
Draw or type your signature, upload a signature image, or capture it with your digital camera.

Share your form instantly
Email, fax, or share your 276277 health care claim form via URL. You can also download, print, or export forms to your preferred cloud storage service.
How to edit 276277 health care claim online
To use the professional PDF editor, follow these steps:
1
Check your account. If you don't have a profile yet, click Start Free Trial and sign up for one.
2
Upload a file. Select Add New on your Dashboard and upload a file from your device or import it from the cloud, online, or internal mail. Then click Edit.
3
Edit 276277 health care claim. Add and replace text, insert new objects, rearrange pages, add watermarks and page numbers, and more. Click Done when you are finished editing and go to the Documents tab to merge, split, lock or unlock the file.
4
Get your file. When you find your file in the docs list, click on its name and choose how you want to save it. To get the PDF, you can save it, send an email with it, or move it to the cloud.
Dealing with documents is always simple with pdfFiller.
Uncompromising security for your PDF editing and eSignature needs
Your private information is safe with pdfFiller. We employ end-to-end encryption, secure cloud storage, and advanced access control to protect your documents and maintain regulatory compliance.
How to fill out 276277 health care claim

How to fill out 276/277 HEALTH CARE CLAIM STATUS REQUEST AND RESPONSE
01
Obtain the 276/277 Health Care Claim Status Request and Response form.
02
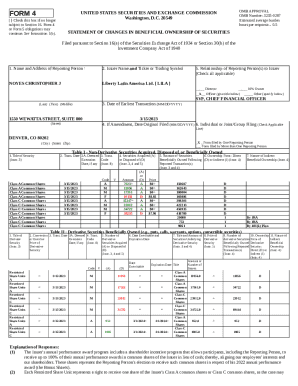
Fill out the required information in the patient section, including the patient's name, date of birth, and insurance details.
03
Provide the claim information, including the claim number and date of service.
04
Indicate the type of status request you are making (e.g., original claim, resubmission).
05
Complete the required provider information, including Provider ID and contact details.
06
Review the filled-out form for accuracy and completeness.
07
Submit the form electronically or via mail, following the specified submission guidelines.
Who needs 276/277 HEALTH CARE CLAIM STATUS REQUEST AND RESPONSE?
01
Health care providers seeking to verify the status of claims submitted to insurance.
02
Insurance companies needing to respond to requests about claim statuses.
03
Billing departments responsible for managing and tracking claims.
Fill
form
: Try Risk Free






People Also Ask about
What is denial 276?
Denial code 276 means that the services rejected by the previous payer are not covered by the current payer.
What is payer rejection code 277?
What is Denial Code 277. Denial code 277 is used when the disposition of a claim or service is undetermined during the premium payment grace period, as required by the Health Insurance SHOP Exchange.
What is a 277 response?
The EDI 277 transaction, also known as a Healthcare Claim Status Notification, is an electronic response sent by an insurance company or payor in reply to an EDI 276 Claim Status Request. It provides healthcare providers with updates on the status of a previously submitted claim.
What is 276 277 claim status response?
The 276 and 277 Transactions are used in tandem: the 276 Transaction is used to inquire about the current status of a specified claim or claims, and the 277 Transaction in response to that inquiry.
What is the denial code 277?
What is Denial Code 277. Denial code 277 is used when the disposition of a claim or service is undetermined during the premium payment grace period, as required by the Health Insurance SHOP Exchange.
What is a 276 transaction in EDI?
The EDI 276 transaction set is a Health Care Claim Status Inquiry. It is used by healthcare providers to verify the status of a claim submitted previously to a payer, such as an insurance company, HMO, government agency like Medicare or Medicaid, etc.
What is the difference between 276 and 277?
The 276 transaction can be received from the trading partner at the line level, but PHC will only be responding at the claim level on the 277 transaction. PHC does not have the functionality to process a line level response. The 276 request is a solicited request that is made by the Trading Partner.
For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
What is 276/277 HEALTH CARE CLAIM STATUS REQUEST AND RESPONSE?
The 276/277 Health Care Claim Status Request and Response is an electronic transaction used in the healthcare industry to inquire about the status of a healthcare claim. It involves sending a request (276) to the payer and receiving a response (277) that provides details regarding the claim's status.
Who is required to file 276/277 HEALTH CARE CLAIM STATUS REQUEST AND RESPONSE?
Health care providers, billing agents, and payers are required to file the 276/277 Health Care Claim Status Request and Response. This includes organizations involved in submitting claims to insurers and those managing claim processes.
How to fill out 276/277 HEALTH CARE CLAIM STATUS REQUEST AND RESPONSE?
To fill out the 276 request, providers must include specific information such as the patient identifier, claim identifier, and necessary transaction details. The response (277) will automatically provide the claim status based on the request submitted.
What is the purpose of 276/277 HEALTH CARE CLAIM STATUS REQUEST AND RESPONSE?
The purpose of the 276/277 transaction is to facilitate communication between providers and payers regarding the status of claims submitted for payment. It helps streamline the claims process, reduces delays, and allows for timely follow-ups on outstanding claims.
What information must be reported on 276/277 HEALTH CARE CLAIM STATUS REQUEST AND RESPONSE?
The 276 request must report information such as the patient ID, claim number, and service date. The 277 response reports claim status indicators, details about payments, adjustments, and any additional remarks related to the claim processing.
Fill out your 276277 health care claim online with pdfFiller!
pdfFiller is an end-to-end solution for managing, creating, and editing documents and forms in the cloud. Save time and hassle by preparing your tax forms online.
276277 Health Care Claim is not the form you're looking for?Search for another form here.
Relevant keywords
Related Forms
If you believe that this page should be taken down, please follow our DMCA take down process
here
.
This form may include fields for payment information. Data entered in these fields is not covered by PCI DSS compliance.