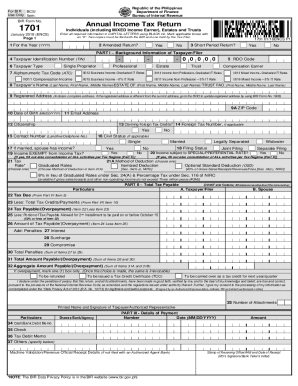
CT ConnectiCare Provider Appeal Request Form 2012-2025 free printable template
Show details
Provider Appeal Request Form Member/Claim Information: Member ID #: Claim #: Member Name: Claim Date of Service: Please give a brief description of why additional payment is warranted: Instructions:
pdfFiller is not affiliated with any government organization
Get, Create, Make and Sign medicare provider appeal request
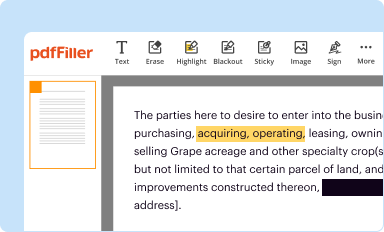
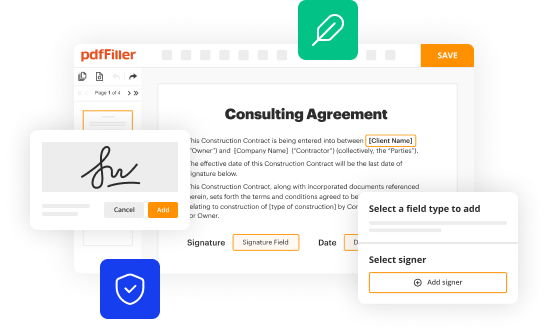
Edit your medicare provider appeal request form online
Type text, complete fillable fields, insert images, highlight or blackout data for discretion, add comments, and more.
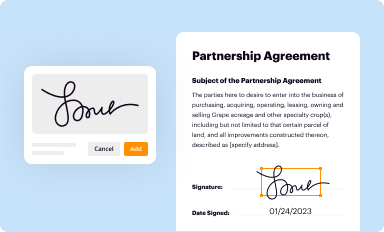
Add your legally-binding signature
Draw or type your signature, upload a signature image, or capture it with your digital camera.
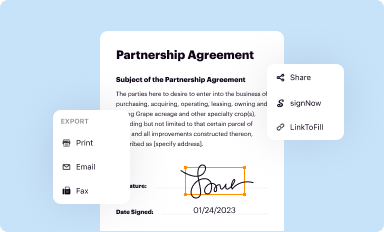
Share your form instantly
Email, fax, or share your medicare provider appeal request form via URL. You can also download, print, or export forms to your preferred cloud storage service.
How to edit medicare provider appeal request online
To use our professional PDF editor, follow these steps:
1
Sign into your account. In case you're new, it's time to start your free trial.
2
Upload a document. Select Add New on your Dashboard and transfer a file into the system in one of the following ways: by uploading it from your device or importing from the cloud, web, or internal mail. Then, click Start editing.
3
Edit medicare provider appeal request. Rearrange and rotate pages, add and edit text, and use additional tools. To save changes and return to your Dashboard, click Done. The Documents tab allows you to merge, divide, lock, or unlock files.
4
Get your file. Select your file from the documents list and pick your export method. You may save it as a PDF, email it, or upload it to the cloud.
pdfFiller makes dealing with documents a breeze. Create an account to find out!
Uncompromising security for your PDF editing and eSignature needs
Your private information is safe with pdfFiller. We employ end-to-end encryption, secure cloud storage, and advanced access control to protect your documents and maintain regulatory compliance.
How to fill out medicare provider appeal request
Point 1: Begin by gathering all necessary documentation and information related to the Medicare claim that you are appealing. This includes the original claim and denial, any supporting medical records, billing documents, and any relevant correspondence.
Point 2: Contact the Medicare Administrative Contractor (MAC) that handles claims for your region. You can find their contact information on the Medicare website or by calling 1-800-MEDICARE. Inform them of your intent to file an appeal and request the necessary forms or guidance on how to submit your appeal.
Point 3: Review the specific requirements and instructions provided by your MAC for filling out the appeal request. Different MACs may have slightly different procedures, so it's important to follow their guidelines to ensure your appeal is properly processed.
Point 4: Complete the appeal request form, providing all requested information accurately and thoroughly. This may include details such as patient information, provider information, claim details, reasons for the appeal, and any supporting documentation you wish to include.
Point 5: Make copies of all completed forms, supporting documents, and correspondence for your own records before submitting them. This will help you keep track of your appeal and provide documentation if needed in the future.
Point 6: Submit your completed appeal request and all supporting documents to the designated address provided by your MAC. It's advisable to send your appeal via certified mail or with a tracking number to ensure delivery and have proof of submission.
Point 7: Keep track of your appeal by noting the date of submission and maintaining regular communication with your MAC. They may request additional information or documentation during the review process, so be prompt in responding to any requests.
Who needs a medicare provider appeal request?
01
Healthcare providers who have had a Medicare claim denied and believe it was unjustified or incorrectly processed.
02
Healthcare providers who have exhausted all other avenues of resolving the claim denial and wish to pursue further action.
03
Healthcare providers who have supporting documentation or evidence to dispute the denial and believe they have a strong case for an appeal.
04
Healthcare providers who are committed to following the proper procedures and requirements set by the MAC to ensure a fair and thorough review of their appeal.
Fill
form
: Try Risk Free






People Also Ask about
What are the five steps in the Medicare appeals process?
The Social Security Act (the Act) establishes five levels to the Medicare appeals process: redetermination, reconsideration, Administrative Law Judge hearing, Medicare Appeals Council review, and judicial review in U.S. District Court.
How do I write an appeal letter to Medicare?
Include this information in your written request: Your name, address, and the Medicare Number on your Medicare card [JPG] The items or services for which you're requesting a reconsideration, the dates of service, and the reason(s) why you're appealing.
What is ConnectiCare Medicare?
ConnectiCare, Inc. is an HMO/HMO-POS plan with a Medicare contract. Enrollment in ConnectiCare depends on contract renewal. ConnectiCare Insurance Company, Inc. is an HMO D-SNP plan with a Medicare contract and a contract with the Connecticut Medicaid Program.
How do I bill ConnectiCare?
By Phone: Call 1-800-224-2273 (TTY: 711) 24 hours a day, seven days a week. Member premium payments go to a bank lockbox. You must include an invoice coupon with the scan line for ConnectiCare to process your payment.
How to fill out Medicare redetermination request form?
A redetermination must be requested in writing.Make a written request containing all of the following information: Beneficiary name. Medicare number. Specific service(s) and/or item(s) for which a redetermination is being requested. Specific date(s) of service. Name of the party, or the representative of the party.
What is the timely filing limit for appeals with ConnectiCare?
Filing limits The filing limit for claims submission is 180 days from the date the services were rendered.
For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
How can I get medicare provider appeal request?
It's simple with pdfFiller, a full online document management tool. Access our huge online form collection (over 25M fillable forms are accessible) and find the medicare provider appeal request in seconds. Open it immediately and begin modifying it with powerful editing options.
How do I complete medicare provider appeal request online?
With pdfFiller, you may easily complete and sign medicare provider appeal request online. It lets you modify original PDF material, highlight, blackout, erase, and write text anywhere on a page, legally eSign your document, and do a lot more. Create a free account to handle professional papers online.
Can I edit medicare provider appeal request on an iOS device?
Create, edit, and share medicare provider appeal request from your iOS smartphone with the pdfFiller mobile app. Installing it from the Apple Store takes only a few seconds. You may take advantage of a free trial and select a subscription that meets your needs.
What is medicare provider appeal request?
A medicare provider appeal request is a request made by a healthcare provider to challenge a decision made by the Centers for Medicare & Medicaid Services (CMS) regarding reimbursement or coverage for medical services.
Who is required to file medicare provider appeal request?
Healthcare providers who have had a claim denied or have received an unfavorable decision from CMS are required to file a medicare provider appeal request.
How to fill out medicare provider appeal request?
To fill out a medicare provider appeal request, the healthcare provider must provide detailed information about the patient, the medical services provided, the reason for the denial, and any supporting documentation.
What is the purpose of medicare provider appeal request?
The purpose of a medicare provider appeal request is to request a review of the decision made by CMS regarding reimbursement or coverage for medical services.
What information must be reported on medicare provider appeal request?
Information that must be reported on a medicare provider appeal request includes patient information, details of the services provided, reason for the denial, and any supporting documentation.
Fill out your medicare provider appeal request online with pdfFiller!
pdfFiller is an end-to-end solution for managing, creating, and editing documents and forms in the cloud. Save time and hassle by preparing your tax forms online.

Medicare Provider Appeal Request is not the form you're looking for?Search for another form here.
Relevant keywords
Related Forms
If you believe that this page should be taken down, please follow our DMCA take down process
here
.
This form may include fields for payment information. Data entered in these fields is not covered by PCI DSS compliance.