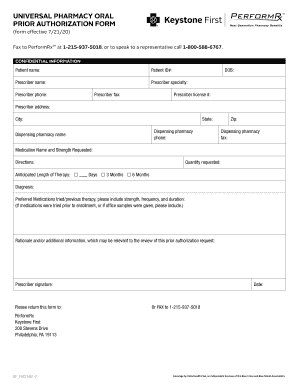
Keystone First Universal Pharmacy Oral Prior Authorization Form free printable template
Show details
Universal Pharmacy Oral Prior Authorization Form
Confidential Information
Patient Name
Patient ID NumberPhysician Name
PhoneSpecialty
License #Physician Address
CityStateZipMedication Name and Strength
pdfFiller is not affiliated with any government organization
Get, Create, Make and Sign keystone first prior auth
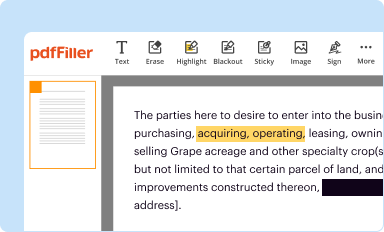
Edit your keystone first prior auth form online
Type text, complete fillable fields, insert images, highlight or blackout data for discretion, add comments, and more.
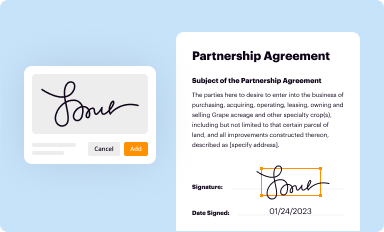
Add your legally-binding signature
Draw or type your signature, upload a signature image, or capture it with your digital camera.
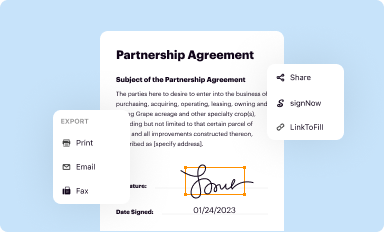
Share your form instantly
Email, fax, or share your keystone first prior auth form via URL. You can also download, print, or export forms to your preferred cloud storage service.
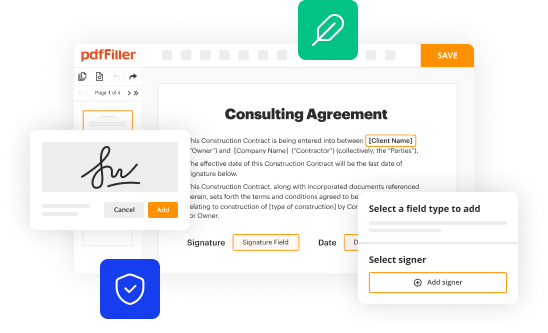
Editing keystone first prior auth online
Here are the steps you need to follow to get started with our professional PDF editor:
1
Set up an account. If you are a new user, click Start Free Trial and establish a profile.
2
Prepare a file. Use the Add New button to start a new project. Then, using your device, upload your file to the system by importing it from internal mail, the cloud, or adding its URL.
3
Edit keystone first prior auth. Add and replace text, insert new objects, rearrange pages, add watermarks and page numbers, and more. Click Done when you are finished editing and go to the Documents tab to merge, split, lock or unlock the file.
4
Get your file. Select your file from the documents list and pick your export method. You may save it as a PDF, email it, or upload it to the cloud.
With pdfFiller, it's always easy to work with documents.
Uncompromising security for your PDF editing and eSignature needs
Your private information is safe with pdfFiller. We employ end-to-end encryption, secure cloud storage, and advanced access control to protect your documents and maintain regulatory compliance.
Keystone First Universal Pharmacy Oral Prior Authorization Form Form Versions
Version
Form Popularity
Fillable & printabley
How to fill out keystone first prior auth
How to fill out Keystone First Universal Pharmacy Oral Prior Authorization
01
Obtain the Keystone First Universal Pharmacy Oral Prior Authorization form.
02
Fill in the patient's personal information, including name, date of birth, and insurance details.
03
Provide details about the medication, including name, dosage, and frequency.
04
Include the prescriber's information, including name, contact number, and licensing details.
05
Attach any relevant clinical information or supporting documentation that justifies the need for the medication.
06
Review the completed form for accuracy and completeness.
07
Submit the form to the appropriate Keystone First contact, following submission guidelines.
Who needs Keystone First Universal Pharmacy Oral Prior Authorization?
01
Patients who require specific medications not typically covered under their health plan.
02
Prescribers submitting requests for medications that may need additional approval.
03
Healthcare providers assisting patients with medication management.
04
Pharmacists involved in processing and aligning prescriptions with health plan requirements.
Fill
form
: Try Risk Free






People Also Ask about
How do I write a prior authorization request?
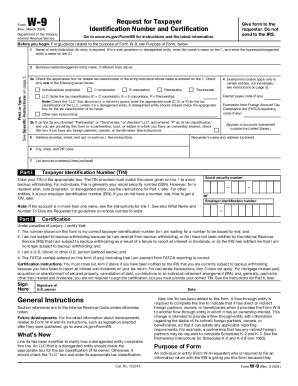
The following information is generally required for all prior authorization letters. The demographic information of the patient (name, date of birth, insurance ID number and more) Provider information (both referring and servicing provider) Requested service/procedure along with specific CPT/HCPCS codes.
How can I make my prior authorization easier?
16 Tips That Speed Up The Prior Authorization Process Create a master list of procedures that require authorizations. Document denial reasons. Sign up for payor newsletters. Stay informed of changing industry standards. Designate prior authorization responsibilities to the same staff member(s).
Why is it so hard to get a prior authorization?
Insurance companies can deny a request for prior authorization for reasons such as: The doctor or pharmacist didn't complete the necessary steps. Filling the wrong paperwork or missing information such as service code or date of birth.
Can you speed up a prior authorization?
Once approved, the prior authorization lasts for a defined timeframe. You may be able to speed up a prior authorization by filing an urgent request. If you can't wait for approval, you may be able to pay upfront at your pharmacy and submit a reimbursement claim after approval.
Does Keystone First require prior authorization?
Pharmacy prior authorizations are required for pharmaceuticals that are not in the formulary, not normally covered, or which have been indicated as requiring prior authorization. For more information on the pharmacy prior authorization process, call the Pharmacy Services department at 1-800-588-6767.
What is the phone number for Keystone First Medicaid prior authorization?
If you have questions about this tool or a service or to request a prior authorization, call 1-800-521-6622.
For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
How do I edit keystone first prior auth in Chrome?
keystone first prior auth can be edited, filled out, and signed with the pdfFiller Google Chrome Extension. You can open the editor right from a Google search page with just one click. Fillable documents can be done on any web-connected device without leaving Chrome.
Can I create an electronic signature for signing my keystone first prior auth in Gmail?
You may quickly make your eSignature using pdfFiller and then eSign your keystone first prior auth right from your mailbox using pdfFiller's Gmail add-on. Please keep in mind that in order to preserve your signatures and signed papers, you must first create an account.
How do I edit keystone first prior auth straight from my smartphone?
The pdfFiller mobile applications for iOS and Android are the easiest way to edit documents on the go. You may get them from the Apple Store and Google Play. More info about the applications here. Install and log in to edit keystone first prior auth.
What is Keystone First Universal Pharmacy Oral Prior Authorization?
Keystone First Universal Pharmacy Oral Prior Authorization is a process used to obtain approval for specific prescription medications before they can be dispensed to patients. It ensures that the medication is clinically necessary and covered by the insurance plan.
Who is required to file Keystone First Universal Pharmacy Oral Prior Authorization?
Healthcare providers or prescribers initiating a prescription for a medication that requires prior authorization must file the Keystone First Universal Pharmacy Oral Prior Authorization.
How to fill out Keystone First Universal Pharmacy Oral Prior Authorization?
To fill out the Keystone First Universal Pharmacy Oral Prior Authorization, healthcare providers must complete a form that includes patient information, prescriber information, medication details, and clinical justification for the requested drug.
What is the purpose of Keystone First Universal Pharmacy Oral Prior Authorization?
The purpose of the Keystone First Universal Pharmacy Oral Prior Authorization is to manage medication costs, ensure appropriate use of medications, and protect patient safety by requiring additional information before approving drug coverage.
What information must be reported on Keystone First Universal Pharmacy Oral Prior Authorization?
The information that must be reported includes the patient's demographic information, the prescriber's contact details, the prescribed medication and dosage, along with clinical rationale, previous treatments tried, and relevant medical history.
Fill out your keystone first prior auth online with pdfFiller!
pdfFiller is an end-to-end solution for managing, creating, and editing documents and forms in the cloud. Save time and hassle by preparing your tax forms online.

Keystone First Prior Auth is not the form you're looking for?Search for another form here.
Relevant keywords
Related Forms
If you believe that this page should be taken down, please follow our DMCA take down process
here
.
This form may include fields for payment information. Data entered in these fields is not covered by PCI DSS compliance.