Get the free Payer Enrollment Instructions
Show details
This document provides detailed instructions for enrolling as a payer with New Hampshire Medicaid, including the use of the Capario portal enrollment tool, required forms, and submission procedures.
We are not affiliated with any brand or entity on this form
Get, Create, Make and Sign payer enrollment instructions
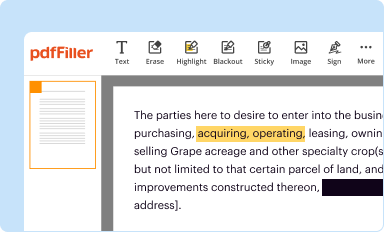
Edit your payer enrollment instructions form online
Type text, complete fillable fields, insert images, highlight or blackout data for discretion, add comments, and more.
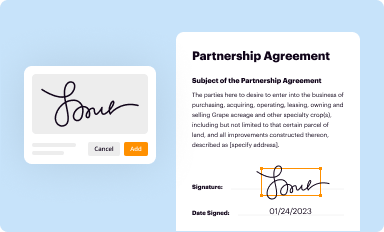
Add your legally-binding signature
Draw or type your signature, upload a signature image, or capture it with your digital camera.
Share your form instantly
Email, fax, or share your payer enrollment instructions form via URL. You can also download, print, or export forms to your preferred cloud storage service.
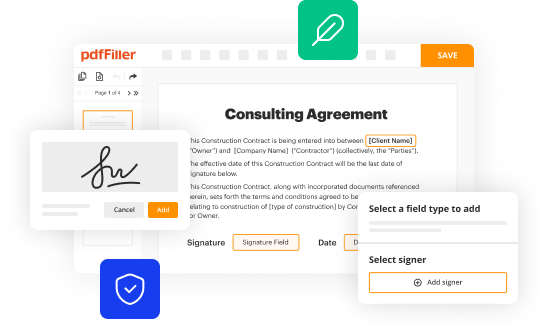
Editing payer enrollment instructions online
To use the professional PDF editor, follow these steps:
1
Log in to your account. Start Free Trial and register a profile if you don't have one yet.
2
Prepare a file. Use the Add New button. Then upload your file to the system from your device, importing it from internal mail, the cloud, or by adding its URL.
3
Edit payer enrollment instructions. Text may be added and replaced, new objects can be included, pages can be rearranged, watermarks and page numbers can be added, and so on. When you're done editing, click Done and then go to the Documents tab to combine, divide, lock, or unlock the file.
4
Get your file. When you find your file in the docs list, click on its name and choose how you want to save it. To get the PDF, you can save it, send an email with it, or move it to the cloud.
pdfFiller makes working with documents easier than you could ever imagine. Register for an account and see for yourself!
Uncompromising security for your PDF editing and eSignature needs
Your private information is safe with pdfFiller. We employ end-to-end encryption, secure cloud storage, and advanced access control to protect your documents and maintain regulatory compliance.
How to fill out payer enrollment instructions
How to fill out Payer Enrollment Instructions
01
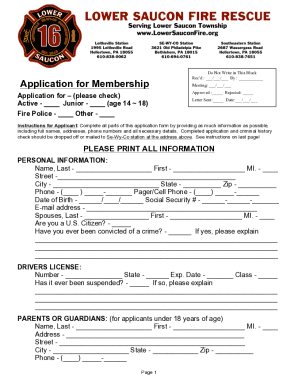
Obtain the Payer Enrollment Instructions form from the relevant payer's website or office.
02
Fill out the required personal information at the top of the form, including name, address, and contact details.
03
Provide your tax identification number or social security number as required.
04
Indicate the type of services you provide or the specialty you fall under.
05
Complete any additional sections required for specific services or enrollment types.
06
Review the form to ensure all information is accurate and complete.
07
Sign and date the form where indicated.
08
Submit the form according to the payer's submission guidelines, whether online, via mail, or fax.
Who needs Payer Enrollment Instructions?
01
Healthcare providers seeking to bill a payer for services rendered.
02
Facilities and institutions that require reimbursement for patient care.
03
Organizations that operate under specific payer agreements for services.
Fill
form
: Try Risk Free






People Also Ask about
What is the provider enrollment process?
Provider Enrollment (or Payor Enrollment) refers to the process of applying to health insurance networks for inclusion in their provider panels. For Commercial Insurance networks, this process involves two steps, 1) Credentialing and 2) Contracting.
What is the difference between provider enrollment specialist and credentialing specialist?
Timing: Provider credentialing is typically done before a healthcare provider is allowed to participate in an insurance network, while provider enrollment is done after a healthcare provider has been approved to participate in an insurance network.
What is a payer enrollment job description?
Coordinates and assists in the enrollment, re-enrollment, re-validation and submission of data/documents for providers and locations in order for them to submit claims for payment. Tracks, monitors and communicates with all payers regarding the status of provider enrollment or termination if necessary.
What is the difference between credentialing and payor enrollment?
What is payer enrollment vs. credentialing. While medical credentialing is an essential process to certify a provider's qualifications, payer enrollment is the process of requesting participation in a health insurance network as a medical provider.
What is the difference between credentialing and payer enrollment?
While medical credentialing is an essential process to certify a provider's qualifications, payer enrollment is the process of requesting participation in a health insurance network as a medical provider.
What are the three types of credentialing?
What is an Example of Credentialing? Professional Credentialing. Facility Credentialing. Payer Enrollment Credentialing.
What is payer enrollment in healthcare?
Payer enrollment is the process of a provider joining a health insurance plan's network. The process includes requesting participation in a payer network, completing credentialing requirements, submitting documents to the payer, and signing a contract.
Can providers see patients before payer credentialing is done?
Seeing patients without payer credentialing being done leads is risky, and providers may face legal issues. If something goes wrong while providing medical services, providers do not have any legal protection and have to face malpractice claims. Liability issues can even result in the termination of their license.
How to do payer enrollment?
Payer Enrollment Process Provider onboards and starts the credentialing process as a new clinician. Provider informs the payer that they are interested in credentialing. Provider manually completes a variety of forms. Payer receives a provider's application. The 90-to-180-day review process begins.
What is the difference between credential and enrollment?
Provider enrollment is distinct from credentialing, although the two processes are often interrelated. While credentialing focuses on verifying the qualifications and competence of the provider, enrollment is about establishing the provider's eligibility to bill a particular payer.
For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
What is Payer Enrollment Instructions?
Payer Enrollment Instructions are guidelines provided to entities that facilitate the enrollment of healthcare providers with insurance payers, allowing them to receive reimbursements for services rendered.
Who is required to file Payer Enrollment Instructions?
Healthcare providers and organizations that wish to bill insurance payers for services must file Payer Enrollment Instructions.
How to fill out Payer Enrollment Instructions?
To fill out Payer Enrollment Instructions, gather necessary information such as provider details, tax identification numbers, and relevant financial information. Follow the provided guidelines and complete all required sections accurately.
What is the purpose of Payer Enrollment Instructions?
The purpose of Payer Enrollment Instructions is to ensure that healthcare providers are properly registered with payers, facilitating timely reimbursement for services and ensuring compliance with payer requirements.
What information must be reported on Payer Enrollment Instructions?
Payer Enrollment Instructions typically require reporting provider identification information, tax identification numbers, bank account details for payments, and any relevant clinical credentials or certifications.
Fill out your payer enrollment instructions online with pdfFiller!
pdfFiller is an end-to-end solution for managing, creating, and editing documents and forms in the cloud. Save time and hassle by preparing your tax forms online.

Payer Enrollment Instructions is not the form you're looking for?Search for another form here.
Relevant keywords
Related Forms
If you believe that this page should be taken down, please follow our DMCA take down process
here
.
This form may include fields for payment information. Data entered in these fields is not covered by PCI DSS compliance.