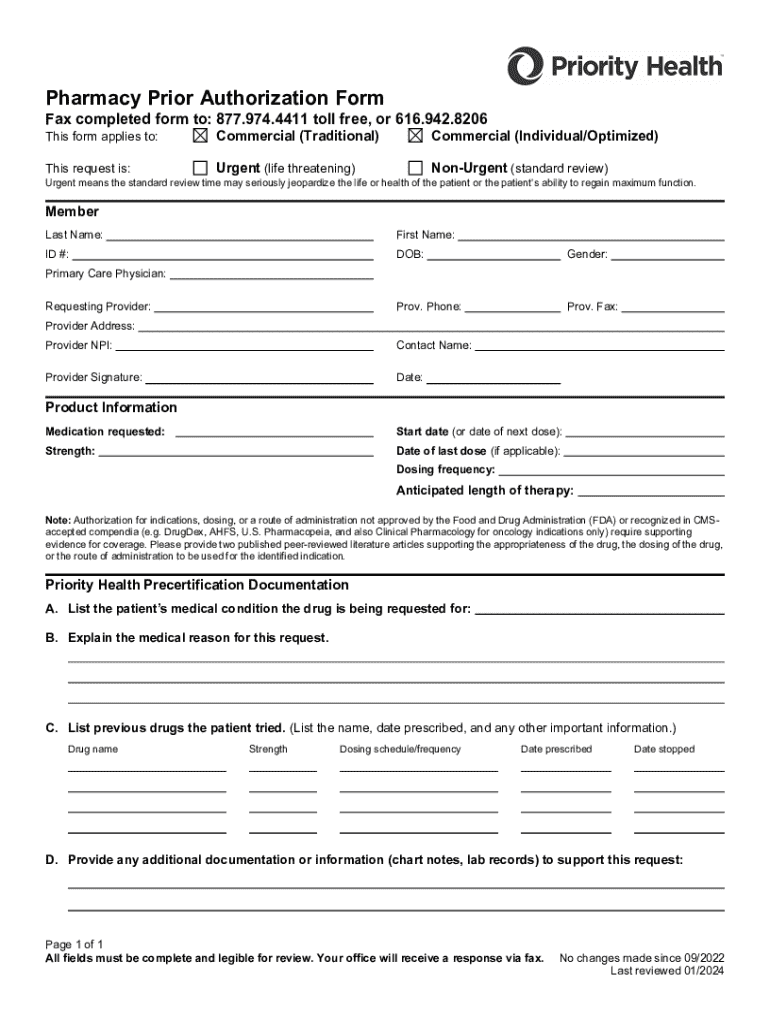
Priority Health Pharmacy Prior Authorization Form 2024-2026 free printable template
Show details
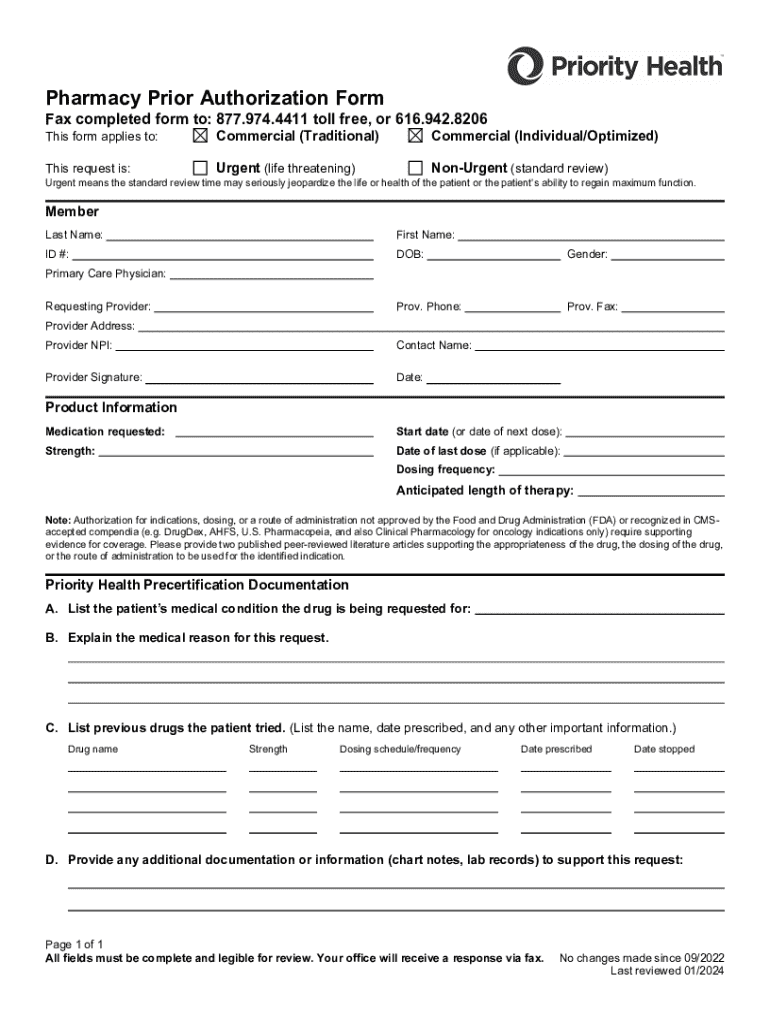
This form is used to request prior authorization for medications for patients covered under commercial insurance plans. It includes sections for patient and provider information, medication details,
pdfFiller is not affiliated with any government organization
Get, Create, Make and Sign Priority Health Pharmacy Prior Authorization Form

Edit your Priority Health Pharmacy Prior Authorization Form form online
Type text, complete fillable fields, insert images, highlight or blackout data for discretion, add comments, and more.

Add your legally-binding signature
Draw or type your signature, upload a signature image, or capture it with your digital camera.

Share your form instantly
Email, fax, or share your Priority Health Pharmacy Prior Authorization Form form via URL. You can also download, print, or export forms to your preferred cloud storage service.
Editing Priority Health Pharmacy Prior Authorization Form online
Use the instructions below to start using our professional PDF editor:
1
Register the account. Begin by clicking Start Free Trial and create a profile if you are a new user.
2
Upload a document. Select Add New on your Dashboard and transfer a file into the system in one of the following ways: by uploading it from your device or importing from the cloud, web, or internal mail. Then, click Start editing.
3
Edit Priority Health Pharmacy Prior Authorization Form. Rearrange and rotate pages, add new and changed texts, add new objects, and use other useful tools. When you're done, click Done. You can use the Documents tab to merge, split, lock, or unlock your files.
4
Save your file. Choose it from the list of records. Then, shift the pointer to the right toolbar and select one of the several exporting methods: save it in multiple formats, download it as a PDF, email it, or save it to the cloud.
With pdfFiller, it's always easy to work with documents.
Uncompromising security for your PDF editing and eSignature needs
Your private information is safe with pdfFiller. We employ end-to-end encryption, secure cloud storage, and advanced access control to protect your documents and maintain regulatory compliance.
Priority Health Pharmacy Prior Authorization Form Form Versions
Version
Form Popularity
Fillable & printabley
Fill
form
: Try Risk Free






People Also Ask about
Is Priority Health only in Michigan?
Your Priority Health insurance can be used at any outside of Michigan facility. However, your provider may not be aware of Priority Health if they are located outside of Michigan.
Does Priority Health have an HSA?
PriorityHSASM is a high-deductible health plan that allows your employees to use a health savings account (HSA) to help pay for medical expenses. The money in the savings account can be used at any time for eligible expenses not paid by the plan. Anyone can contribute to it, including you as an employer.
How can I make my prior authorization faster?
16 Tips That Speed Up The Prior Authorization Process Create a master list of procedures that require authorizations. Document denial reasons. Sign up for payor newsletters. Stay informed of changing industry standards. Designate prior authorization responsibilities to the same staff member(s).
How does pre authorization work?
Prior authorization (also called “preauthorization” and “precertification”) refers to a requirement by health plans for patients to obtain approval of a health care service or medication before the care is provided. This allows the plan to evaluate whether care is medically necessary and otherwise covered.
What does it mean to need a prior authorization for a medication?
What is prior authorization? This means we need to review some medications before your plan will cover them. We want to know if the medication is medically necessary and appropriate for your situation. If you don't get prior authorization, a medication may cost you more, or we may not cover it.
Is Priority Health accepted in Texas?
What should I do? A: Your Priority Health insurance can be used at any outside of Michigan facility in the U.S. However, your provider may not be familiar with Priority Health if they are located outside of Michigan.
Which procedure is most likely to need a prior authorization?
What Procedures or Tests Typically Require Prior Approval? Diagnostic imaging such as MRIs, CTs and PET scans. Durable medical equipment such as wheelchairs, at-home oxygen and patient lifts. Infusion therapy. Inpatient procedures. Skilled nursing visits and other home health care.
Is Priority Medicare a Medicare Advantage Plan?
Priority Health offers Medicare Advantage with prescription drug plans (MAPD) and Medigap (Medicare Supplement) plans.
Why would a prior authorization be needed?
Prior authorization (also called “preauthorization” and “precertification”) refers to a requirement by health plans for patients to obtain approval of a health care service or medication before the care is provided. This allows the plan to evaluate whether care is medically necessary and otherwise covered.
What is an example of prior authorization?
For example, your health plan may require prior authorization for an MRI, so that they can make sure that a lower-cost x-ray wouldn't be sufficient. The service isn't being duplicated: This is a concern when multiple specialists are involved in your care.
What types of medications may require a prior authorization?
What types of prescriptions require prior authorizations? Insurance companies will most likely require prior authorizations for the following drugs: Brand-name drugs that have a generic available. Drugs that are intended for certain age groups or conditions only.
What is a prior authorization form for medication?
What is a Prior Authorization? A prior authorization (PA), sometimes referred to as a “pre-authorization,” is a requirement from your health insurance company that your doctor obtain approval from your plan before it will cover the costs of a specific medicine, medical device or procedure.
How long do pre authorizations take?
How Does Prior Authorization Work? Most in-network providers submit a prior authorization request on your behalf. Still, it's always a good idea to check with your provider or a Personal Health Guide to ensure a particular procedure or service is approved. Prior authorization typically takes 7–14 business days.
For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
How do I modify my Priority Health Pharmacy Prior Authorization Form in Gmail?
pdfFiller’s add-on for Gmail enables you to create, edit, fill out and eSign your Priority Health Pharmacy Prior Authorization Form and any other documents you receive right in your inbox. Visit Google Workspace Marketplace and install pdfFiller for Gmail. Get rid of time-consuming steps and manage your documents and eSignatures effortlessly.
How can I edit Priority Health Pharmacy Prior Authorization Form on a smartphone?
The pdfFiller apps for iOS and Android smartphones are available in the Apple Store and Google Play Store. You may also get the program at https://edit-pdf-ios-android.pdffiller.com/. Open the web app, sign in, and start editing Priority Health Pharmacy Prior Authorization Form.
How do I edit Priority Health Pharmacy Prior Authorization Form on an iOS device?
You certainly can. You can quickly edit, distribute, and sign Priority Health Pharmacy Prior Authorization Form on your iOS device with the pdfFiller mobile app. Purchase it from the Apple Store and install it in seconds. The program is free, but in order to purchase a subscription or activate a free trial, you must first establish an account.
What is pharmacy prior authorization form?
A pharmacy prior authorization form is a document that a healthcare provider submits to a health insurance company to obtain approval for a specific medication before it can be prescribed to a patient.
Who is required to file pharmacy prior authorization form?
Typically, the healthcare provider who is prescribing the medication is required to file the pharmacy prior authorization form, with assistance from the patient's pharmacy or the patient as needed.
How to fill out pharmacy prior authorization form?
To fill out a pharmacy prior authorization form, the healthcare provider should include patient information, medication details, reason for the requested medication, past treatments, and additional clinical information that supports the need for the medication.
What is the purpose of pharmacy prior authorization form?
The purpose of a pharmacy prior authorization form is to ensure that the prescribed medication is medically necessary, to control costs, and to verify that the patient meets specific criteria set by the insurance provider for coverage.
What information must be reported on pharmacy prior authorization form?
The information that must be reported on a pharmacy prior authorization form typically includes patient demographics, prescribing physician information, medication being requested, diagnosis, treatment history, and supporting clinical information.
Fill out your Priority Health Pharmacy Prior Authorization Form online with pdfFiller!
pdfFiller is an end-to-end solution for managing, creating, and editing documents and forms in the cloud. Save time and hassle by preparing your tax forms online.
Priority Health Pharmacy Prior Authorization Form is not the form you're looking for?Search for another form here.
Relevant keywords
Related Forms
If you believe that this page should be taken down, please follow our DMCA take down process
here
.
This form may include fields for payment information. Data entered in these fields is not covered by PCI DSS compliance.