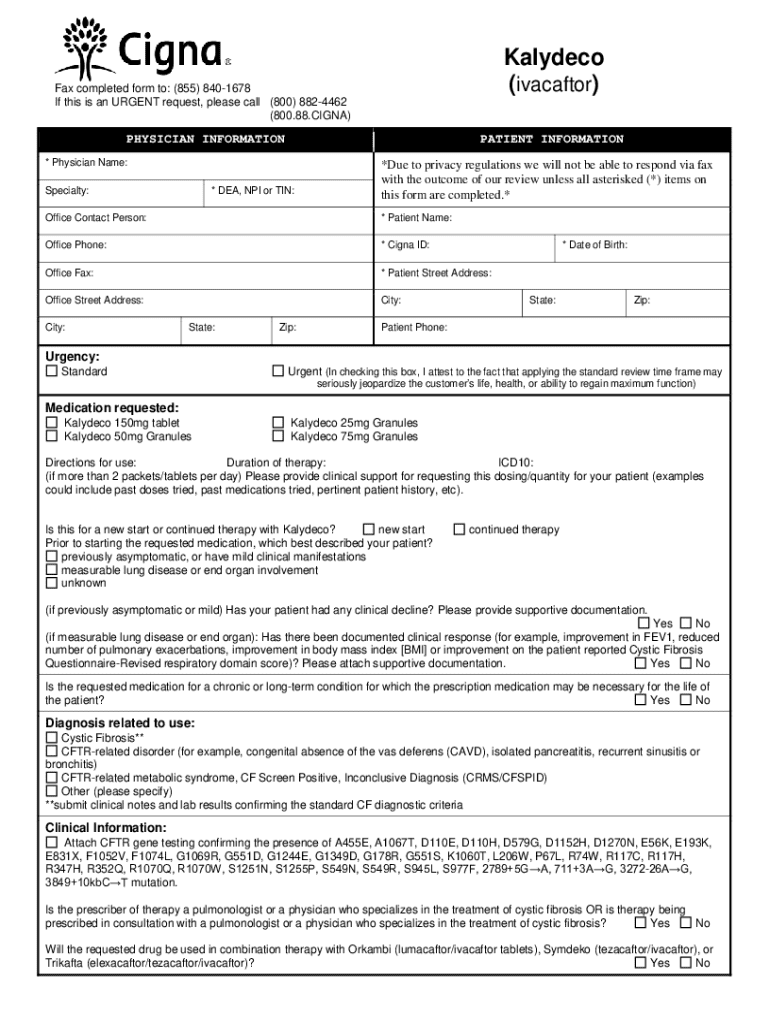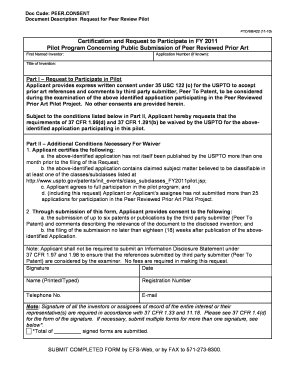
Get the free Kalydeco Prior Authorization Form
Get, Create, Make and Sign kalydeco prior authorization form



How to edit kalydeco prior authorization form online
Uncompromising security for your PDF editing and eSignature needs
How to fill out kalydeco prior authorization form

How to fill out kalydeco prior authorization form
Who needs kalydeco prior authorization form?
Kalydeco Prior Authorization Form: A Comprehensive Guide
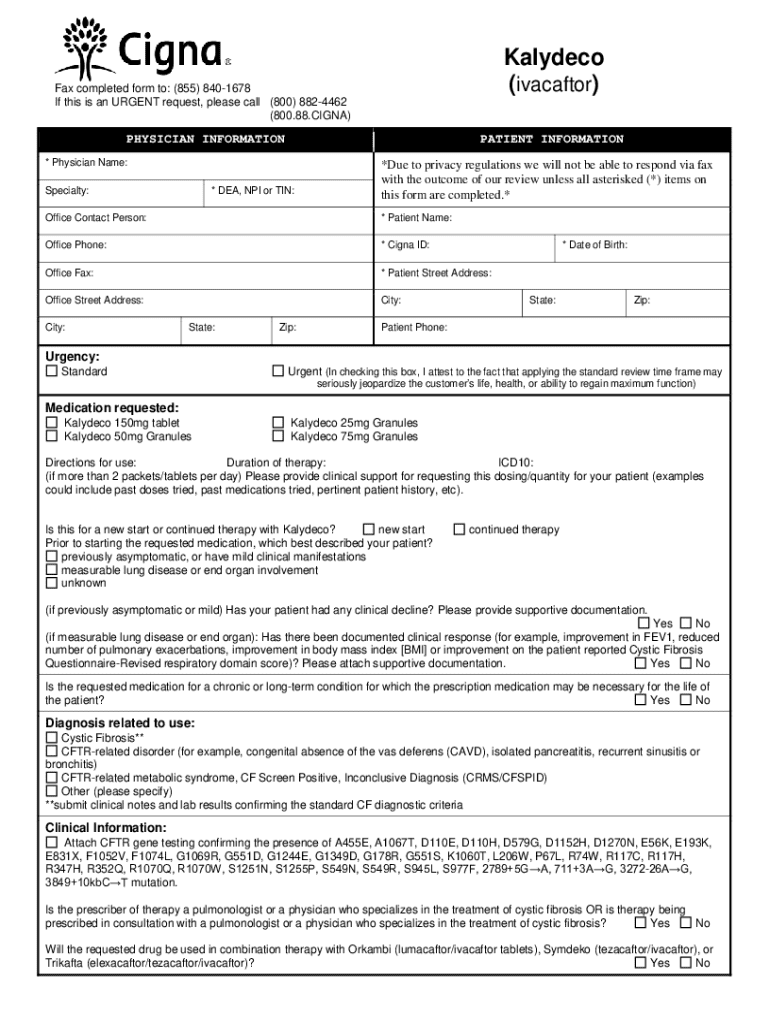
Overview of Kalydeco
Kalydeco (ivacaftor) is a groundbreaking medication designed to treat cystic fibrosis in patients aged six months and older who have a specific genetic mutation. It works by improving the function of the defective protein that causes the disease, thereby helping to enhance lung function and reduce associated complications. As a specialty drug with a high cost, Kalydeco requires prior authorization from insurance providers to ensure coverage for patients, making the understanding of the kalydeco prior authorization form essential.
The importance of prior authorization stems from the necessity to confirm that Kalydeco is medically appropriate and aligns with the treatment guidelines. Prior authorization not only helps to manage healthcare costs but also ensures that patients receive the most effective treatments for their conditions. Kalydeco is primarily utilized for treating cystic fibrosis stemming from G551D and other specific mutations in the CFTR gene.
Understanding prior authorization
Prior authorization is a process utilized by insurance companies to determine if a prescription medication is medically necessary before providing coverage. The goal is to ensure that patients receive appropriate care, mitigating unnecessary expenses. For Kalydeco, the prior authorization process serves as a checkpoint that encourages physicians to provide comprehensive evidence to support the use of this drug.
The necessity of prior authorization for Kalydeco arises from the drug's specialized nature and its associated costs. Insurance companies want to ensure that the prescribed treatment aligns with clinical guidelines and patient-specific circumstances. Key stakeholders in this process include patients, who must navigate the complexity of obtaining their medication; healthcare providers, responsible for submitting the request; and insurance companies, tasked with reviewing and approving requests.
The Kalydeco prior authorization process
Navigating the Kalydeco prior authorization process can feel daunting. However, knowing the specific steps involved can simplify the experience. Here's a step-by-step guide to obtaining prior authorization for Kalydeco:
Completing the Kalydeco prior authorization form
Filling out the Kalydeco prior authorization form accurately is crucial for the approval process. The form consists of multiple sections that gather essential information regarding the patient and their treatment. Here’s a detailed breakdown of the form's sections:
To ensure the accuracy of the form, common mistakes to avoid include incomplete information, missing signatures, and neglecting to provide adequate supporting evidence. Verifying the completed form with your healthcare provider can improve your chances of a successful submission.
Follow-up and tracking your request
After submitting the Kalydeco prior authorization form, the next step involves following up on the request. Patients should inquire with their healthcare provider or directly with the insurance company to verify that the request is being processed. It's essential to know how to check the status of your prior authorization request, typically available through customer service channels or online portals provided by the insurance company.
In the unfortunate event that your request is denied, understanding the reasons behind the denial is crucial. This understanding allows for a more informed approach to appeals and resubmission. The process includes reviewing feedback from the insurance company, addressing the stated concerns, and potentially providing additional documentation to support the case.
Frequently asked questions (FAQs) about Kalydeco prior authorization
Patients often have questions regarding the prior authorization process for Kalydeco. Here are some frequently asked questions:
Using pdfFiller for editing and managing your Kalydeco prior authorization form
pdfFiller enhances the experience of managing the Kalydeco prior authorization requests. The platform allows users to create, edit, and eSign the required documents in a cloud-based environment, fostering seamless collaboration.
Key features of pdfFiller include:
Troubleshooting common issues with Kalydeco prior authorization
Challenges are common in the prior authorization process for Kalydeco. These challenges often stem from insufficient documentation, incorrect information, or prolonged waiting periods. To overcome these hurdles, it’s essential to remain organized and proactive.
The resources available within pdfFiller can assist users in managing their documents effectively, from tips on formatting to troubleshooting potential issues. Additionally, contacting customer support for additional help can provide clarity and guidance on resolving any specific challenges encountered during the process.
Real-life cases of Kalydeco prior authorization
Real-life experiences highlight the importance of a thorough and informed approach to prior authorization requests. Many patients have successfully navigated the process with the help of their healthcare providers, illustrating the collaboration necessary for obtaining timely access to Kalydeco.
Lessons learned include the importance of submitting comprehensive documentation and asking for help when needed, particularly from healthcare providers who can effectively advocate on behalf of their patients. Successful stories underscore not only the role of patients but also the critical involvement of healthcare professionals in facilitating the Kalydeco prior authorization process.






For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
How can I manage my kalydeco prior authorization form directly from Gmail?
How do I edit kalydeco prior authorization form online?
How do I complete kalydeco prior authorization form on an Android device?
What is kalydeco prior authorization form?
Who is required to file kalydeco prior authorization form?
How to fill out kalydeco prior authorization form?
What is the purpose of kalydeco prior authorization form?
What information must be reported on kalydeco prior authorization form?
pdfFiller is an end-to-end solution for managing, creating, and editing documents and forms in the cloud. Save time and hassle by preparing your tax forms online.