Get the free Cystic Fibrosis Prior Authorization Request Form
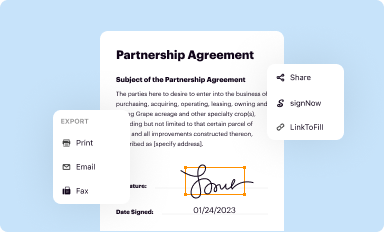
Get, Create, Make and Sign cystic fibrosis prior authorization
How to edit cystic fibrosis prior authorization online
Uncompromising security for your PDF editing and eSignature needs
How to fill out cystic fibrosis prior authorization
How to fill out cystic fibrosis prior authorization
Who needs cystic fibrosis prior authorization?
Cystic Fibrosis Prior Authorization Form: A Comprehensive Guide
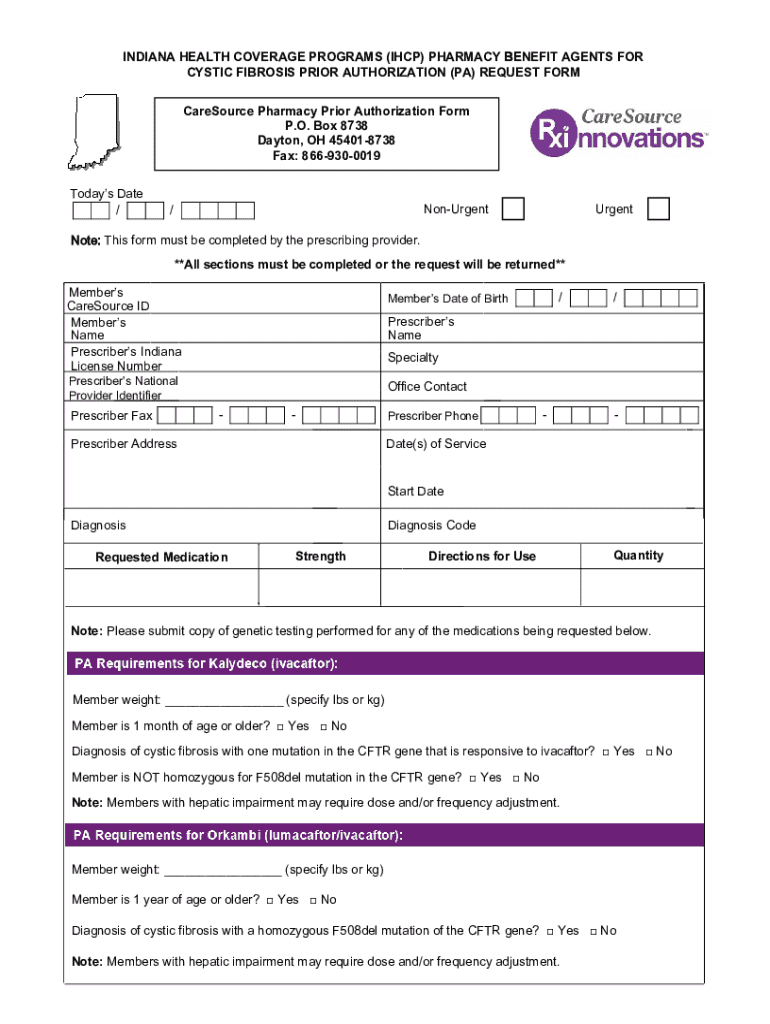
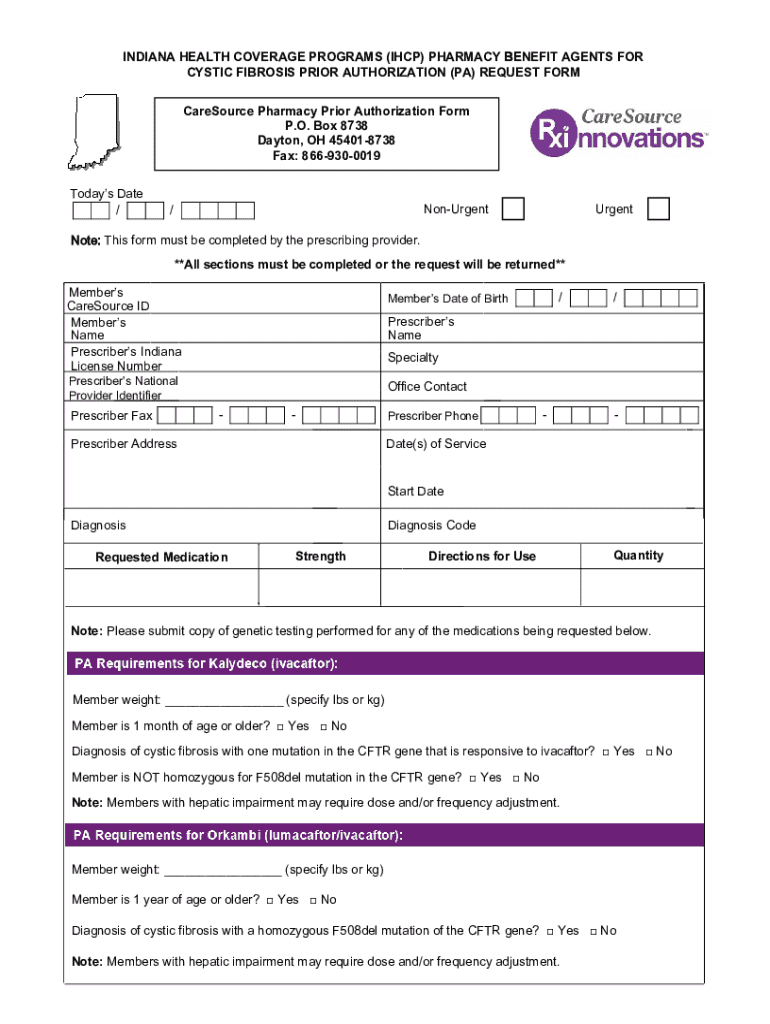
Understanding the cystic fibrosis prior authorization form
A cystic fibrosis prior authorization form is a critical document that healthcare providers must submit to insurance companies before certain treatments or medications can be approved for patients with cystic fibrosis (CF). This form serves as a gateway, ensuring that the prescribed treatments align with a patient’s clinical needs and that they meet the insurer’s criteria for reimbursement. The importance of this process cannot be overstated as it significantly impacts treatment access and timely intervention by healthcare providers for patients dealing with the complexities of cystic fibrosis.
Preparing for the prior authorization process
To effectively navigate the prior authorization process for cystic fibrosis, it’s essential to prepare adequately. A successful submission hinges on having precise and complete information readily available.
Moreover, creating a documentation checklist can significantly streamline this process. Assemble the necessary medical records, lab results, and notes from healthcare providers that justify the need for specific treatments. This approach ensures that the submission is thorough and minimizes delays in approval.
Step-by-step instructions for completing the form
Completing the cystic fibrosis prior authorization form can initially seem daunting. Here’s a detailed guide to help you through each step.
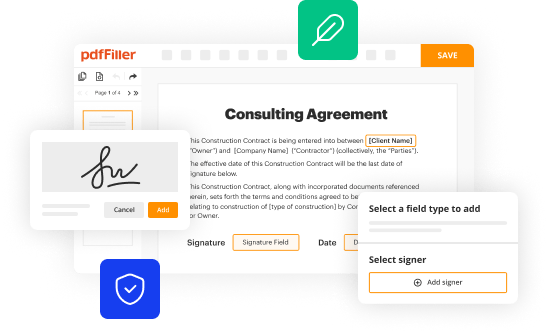
Utilizing the editing tools available on pdfFiller can enhance the form's clarity, allowing for necessary notes to be added and ensuring that all information is coherent before submission.
Reviewing your submission
Before submitting the cystic fibrosis prior authorization form, review your entries meticulously. A simple error can lead to significant delays. PdfFiller offers features that allow you to check the information entered easily.
Editing and managing your form with pdfFiller
PdfFiller provides robust features that facilitate the editing and collaborative review process when handling the cystic fibrosis prior authorization form. These tools are invaluable for streamlining communication between healthcare providers.
Submission process
Once you are confident that the cystic fibrosis prior authorization form is complete, it's time to submit it. Multiple submission methods are available, and knowing the correct one is essential.
Frequently asked questions (FAQs)
The prior authorization process can often lead to various questions. Here are some of the most common inquiries around the cystic fibrosis prior authorization form.
Common scenarios and troubleshooting
Errors during submission of the cystic fibrosis prior authorization form can be frustrating. Knowing how to troubleshoot common issues can save time and effort.
Examining case studies where other patients experienced successful submissions can provide insight into best practices and potential pitfalls.
Additional support and contact information
If you encounter challenges during the prior authorization process, help is available. Contacting support teams related to pdfFiller can expedite resolution.
Benefits of using pdfFiller
PdfFiller is more than just a document management tool; it is an ally in navigating the complexities of the cystic fibrosis prior authorization form. Its numerous features empower users to efficiently manage documents, from collaborative editing to e-signing capabilities.






For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
How do I complete cystic fibrosis prior authorization online?
How do I make edits in cystic fibrosis prior authorization without leaving Chrome?
How do I edit cystic fibrosis prior authorization on an Android device?
What is cystic fibrosis prior authorization?
Who is required to file cystic fibrosis prior authorization?
How to fill out cystic fibrosis prior authorization?
What is the purpose of cystic fibrosis prior authorization?
What information must be reported on cystic fibrosis prior authorization?
pdfFiller is an end-to-end solution for managing, creating, and editing documents and forms in the cloud. Save time and hassle by preparing your tax forms online.