
Get the free Cystic Fibrosis Prior Authorization Request Form - dvha vermont
Get, Create, Make and Sign cystic fibrosis prior authorization
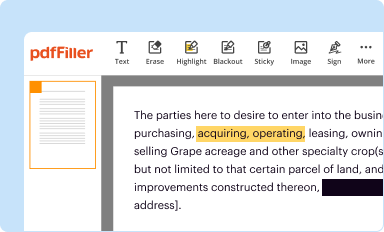
Editing cystic fibrosis prior authorization online
Uncompromising security for your PDF editing and eSignature needs
How to fill out cystic fibrosis prior authorization
How to fill out cystic fibrosis prior authorization
Who needs cystic fibrosis prior authorization?
Cystic fibrosis prior authorization form: A comprehensive guide
Breadcrumb navigation
Home > Forms > Cystic Fibrosis Prior Authorization Form
Understanding the cystic fibrosis prior authorization form
A prior authorization is a crucial step in ensuring that patients receive the medical treatments they need, especially for chronic conditions like cystic fibrosis (CF). This process requires healthcare providers to obtain approval from insurance companies before specific medications or procedures are covered. In the context of cystic fibrosis, prior authorization becomes particularly important due to the high costs associated with CF therapies. By having a structured framework around the prior authorization form, patients can ensure they navigate this necessity with optimal understanding and efficiency.
The importance of prior authorization for cystic fibrosis treatments cannot be overstated; it safeguards patients by ensuring that their prescribed therapies are not only medically necessary but also cost-effective. Many of the advanced treatments available today require prior approval due to their high price tag. Without this authorization, patients may find themselves facing unexpected out-of-pocket costs or even delayed access to essential medications.
Instructions for accessing the form
Locating the cystic fibrosis prior authorization form can vary depending on your health insurance provider. To streamline this process, here’s a step-by-step guide to help you find the form effectively.
The forms may be available in various formats, including PDF for printing or online submission mechanisms. Each format has its pros and cons, depending on personal preference and accessibility needs. For example, PDF forms can be downloaded and filled in at your convenience but may require printing for physical signatures. Online submissions are often quicker and may reduce the risk of lost paperwork but can be less user-friendly if you're not familiar with digital forms.
Detailed sections of the cystic fibrosis prior authorization form
The cystic fibrosis prior authorization form contains several key sections that must be filled out accurately to minimize delays in processing. Each section plays a critical role in the approval process, ensuring that the necessary information is provided to justify the treatment request.
Instructions for completing the form
Completing the cystic fibrosis prior authorization form correctly is essential for ensuring your request is processed smoothly. Here are some tips for accuracy in data entry, along with required documentation to attach.
Navigating the submission process
Submitting the completed cystic fibrosis prior authorization form correctly is just as important as filling it out accurately. Follow these steps for submission to ensure it reaches the right destination.
Frequently asked questions (FAQs)
Many questions arise regarding the cystic fibrosis prior authorization process. Here are some frequently asked questions that can clarify your concerns.
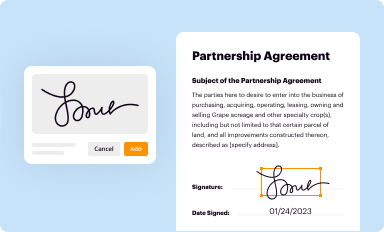
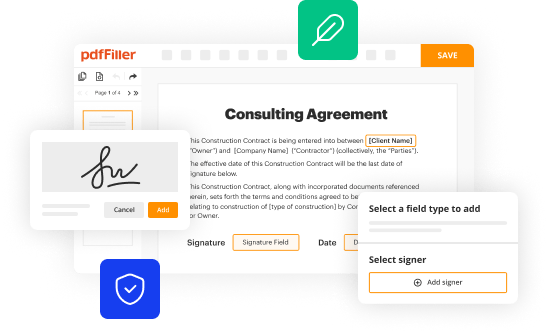
Managing your documentation with pdfFiller
Using pdfFiller streamlines the process of editing, signing, and managing your cystic fibrosis prior authorization form efficiently. With various interactive tools available, users can ensure collaborative efforts are productive.
Additional tips for individuals and teams
Staying organized is vital when managing complex paperwork such as the cystic fibrosis prior authorization form. Here are essential tips to help maintain efficiency.
Contact support for assistance
If you run into any challenges or need further assistance with the cystic fibrosis prior authorization form, reaching out to customer support can provide necessary help and guidance.






For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
Can I create an electronic signature for the cystic fibrosis prior authorization in Chrome?
How do I complete cystic fibrosis prior authorization on an iOS device?
How do I fill out cystic fibrosis prior authorization on an Android device?
What is cystic fibrosis prior authorization?
Who is required to file cystic fibrosis prior authorization?
How to fill out cystic fibrosis prior authorization?
What is the purpose of cystic fibrosis prior authorization?
What information must be reported on cystic fibrosis prior authorization?
pdfFiller is an end-to-end solution for managing, creating, and editing documents and forms in the cloud. Save time and hassle by preparing your tax forms online.















