
Get the free Provider Expedited Appeal Form
Get, Create, Make and Sign provider expedited appeal form
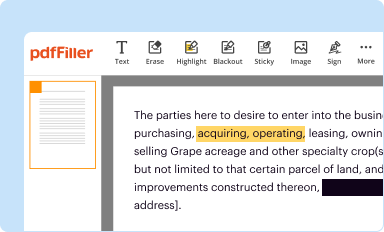
How to edit provider expedited appeal form online
Uncompromising security for your PDF editing and eSignature needs
How to fill out provider expedited appeal form
How to fill out provider expedited appeal form
Who needs provider expedited appeal form?
Provider Expedited Appeal Form: A Comprehensive How-to Guide
Understanding the provider expedited appeal form
The provider expedited appeal form is a crucial document in healthcare that enables healthcare providers to challenge adverse benefit determinations made by insurance companies. It allows a provider to request a swift review of a decision that has the potential to impact patient care significantly. This form plays an essential role in the expedited appeal process, which is designed to address urgent matters in patient treatment when time is of the essence.
When a patient’s treatment is denied or delayed, it often leads to negative health outcomes. Thus, expedited appeals are critical in ensuring that necessary healthcare interventions are not unnecessarily postponed. This appeal process not only safeguards patients' rights but also supports healthcare providers in advocating for their patients, ensuring they receive the appropriate care without breaches in timelines.
Key components of the provider expedited appeal form
Completing the provider expedited appeal form requires several key components to ensure the submission is comprehensive and effective. First, essential information must be accurately filled, including the provider's identification details such as name, NPI number, and contact information. Patient-specific details, including their insurance information and the nature of their condition, are also vital. Additionally, it's crucial to describe the service or treatment being contested.
The reason for the expedited appeal, which must be set forth clearly, is equally essential. Common reasons include situations where a delay could significantly harm the patient’s health or wellbeing. To support your claim, adequate documentation such as medical records, treatment plans, and any relevant literature should be attached.
Step-by-step instructions for completing the provider expedited appeal form
Filling out the provider expedited appeal form can be streamlined by following a series of steps diligently. Start by gathering all required information to avoid delays or incomplete submissions. This includes personalizing the form with precise details, as inaccuracies can lead to the rejection of your appeal.
Next, diligently fill out each section of the form, ensuring that each entry aligns with the insurance provider's stipulations. Be aware of common pitfalls: failing to fill in all mandatory fields or neglecting to sign the form can impede the process. Lastly, review your submission critically. Proofreading tools can aid in this process, ensuring that all data is clear and accurate while emphasizing a concise presentation of your case.
Submitting the provider expedited appeal form
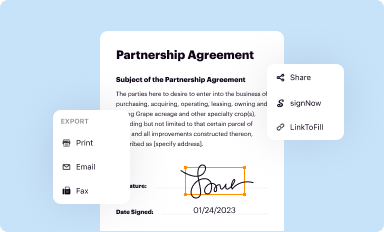
Once completed, knowing where and how to submit the provider expedited appeal form is vital for a successful outcome. Providers can generally submit the form through various methods, including online submission portals, mailing, or faxing directly to the insurance company. Ensure you check the specific submission guidelines set forth by the insurance providers as they may vary.
Tracking your appeal status is crucial after submission. Many insurance companies provide a means to confirm receipt of your appeal, either through online systems or by contacting dedicated units. Understanding how to follow up can keep you informed about the process and any further actions required.
What happens after submission?
Once the provider expedited appeal form is submitted, it enters the review phase. Typically, insurance companies aim to make decisions on expedited appeals swiftly, often within a few days to a couple of weeks. Understanding the review process is vital, as it generally involves assessing the urgency and validity of the appeal based on the submitted documentation.
After the review, you'll receive the outcome of your appeal. It can either be an approval, denial, or a request for more information. Each scenario will define your next steps: If approved, you can proceed with the treatment. If denied, you may have options, such as filing a comprehensive appeal or requesting an external review.
Best practices for filing an expedited appeal
To increase the likelihood of a successful expedited appeal, it's essential to build a strong case. This often means providing substantial supporting documentation that clearly articulates the necessity of the treatment contested. The clarity and detail in your explanations can significantly enhance your appeal's effectiveness, so avoid vague terms and focus on factual, detailed descriptions.
Simultaneously, it's crucial to recognize and avoid common mistakes that could hinder your appeal. Many providers submit incomplete forms or face missed deadlines for submission. Paying attention to these details can make a significant difference in the outcome of your expedited appeal.
Utilizing pdfFiller for managing your provider expedited appeal form
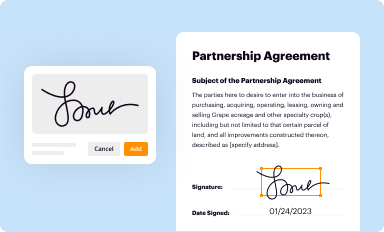
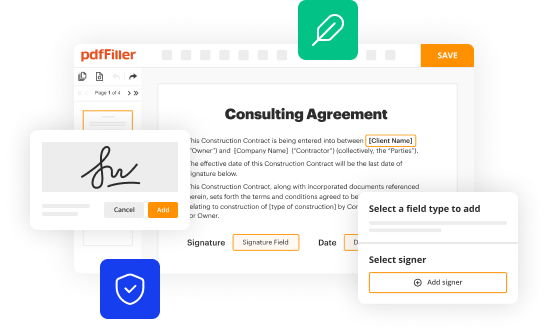
pdfFiller is an excellent tool for managing your provider expedited appeal form, offering a cloud-based document solution that greatly enhances the appeal process. One of the key benefits is the ability to edit PDF forms seamlessly online, which allows for quick adjustments and ensures that all necessary information is accurately represented on the form.
Additionally, pdfFiller facilitates eSigning and enables collaboration among team members, streamlining the workflow considerably. With interactive features for tracking changes and managing multiple revisions, your document management process becomes smoother, more efficient, and secure, allowing healthcare providers to store and access documents anywhere.
Real-life examples and case studies
Examining real-life success stories of expedited appeals can provide invaluable insights for providers. For example, consider a case where a medical practice submitted an expedited appeal for a patient requiring immediate surgery after a denied request. Their thorough documentation, including a detailed medical necessity letter, led to a swift approval, demonstrating the power of a well-articulated case.
On the other hand, analyzing unsuccessful appeals offers lessons worth noting. A common oversight was the omission of essential medical records. This led to denials that could have been prevented with more robust documentation. Learning from these experiences can significantly improve future appeal submissions.
Frequently asked questions (FAQs) about the provider expedited appeal process
As healthcare providers navigate the complexities of the provider expedited appeal form, several common questions arise. Frequently, questions concern the specifics of filling out the form accurately or misunderstandings about the timelines of the review process. Oftentimes, providers seek clarification on what constitutes grounds for an appeal and how to handle unique patient scenarios.
Providing clear answers to these questions ensures that providers feel equipped to tackle the appeal process. Guidance on best practices, and regular communication with insurance representatives can demystify the process, empowering healthcare professionals to pursue their patients' rights effectively.






For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
How can I get provider expedited appeal form?
How do I edit provider expedited appeal form in Chrome?
How do I edit provider expedited appeal form on an Android device?
What is provider expedited appeal form?
Who is required to file provider expedited appeal form?
How to fill out provider expedited appeal form?
What is the purpose of provider expedited appeal form?
What information must be reported on provider expedited appeal form?
pdfFiller is an end-to-end solution for managing, creating, and editing documents and forms in the cloud. Save time and hassle by preparing your tax forms online.






















