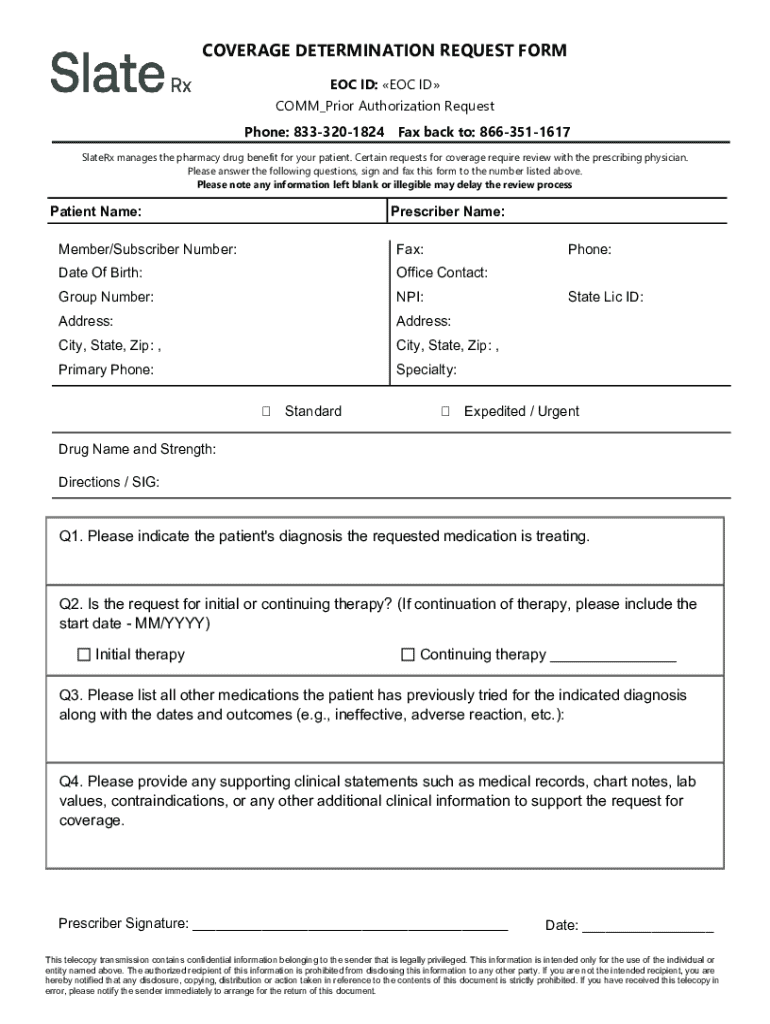
Get the free Coverage Determination Request Form
Get, Create, Make and Sign coverage determination request form
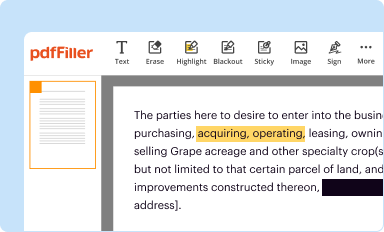
How to edit coverage determination request form online
Uncompromising security for your PDF editing and eSignature needs
How to fill out coverage determination request form
How to fill out coverage determination request form
Who needs coverage determination request form?
A Comprehensive Guide to the Coverage Determination Request Form
Understanding the coverage determination request form
The coverage determination request form serves as a pivotal document in the healthcare landscape, particularly within the insurance process. It is primarily used by patients and healthcare providers to formally request coverage for specific treatments, medications, or procedures that may not be routinely covered under an insurance policy.
This form is essential because it provides a structured means for individuals to seek necessary healthcare services that are otherwise not included in their insurance plan. By submitting this form, patients can clarify their needs and justify why certain treatments should be covered, resulting in a smoother claims process.
Key components of the form
Who should use the coverage determination request form?
The target audience for the coverage determination request form is two-fold: patients and healthcare providers. Patients looking to cover specific treatments or medications that are not typically included in their insurance plans are the primary users of this document. Healthcare providers act as facilitators, helping patients navigate the complexities of insurance coverage and ensuring that all necessary information is accurately presented.
Using this form becomes necessary in various scenarios, such as when a patient's prescribed medication is deemed non-formulary by their insurance or when a certain procedure requires pre-authorization. Examples include requesting post-operative rehabilitation therapy or an experimental treatment not covered by an insurance policy.
Step-by-step guide to filling out the coverage determination request form
Step 1: Gather necessary information
Before filling out the form, make sure to gather relevant information. This includes the patient's medical history, details about the treatment or medication in question, and insurance policy information, such as the coverage terms and benefit exclusions. Comprehensive knowledge of existing medical records can bolster the request’s chances for approval.
Step 2: Completing the form accurately
Accuracy is critical when completing the coverage determination request form. Each section should be filled with attention to detail.
Step 3: Reviewing your submission
Reviewing your submission is essential. Double-check for any errors that may invalidate your request. Common errors include misspelled names, incorrect dates or missing signatures. Ensuring the accuracy of the form can expedite processing and prevent unnecessary delays.
Submitting the coverage determination request form
The next crucial step after completing the coverage determination request form is submission. There are generally two accepted methods for submitting this document.
After submission, it is wise to track your request. Following up with your insurer can keep you informed about the status of your coverage determination. The standard timelines for processing requests can vary, typically ranging from a few days to several weeks.
What happens after submission?
After submitting the coverage determination request form, it enters a review process where the insurance company evaluates the request based on the provided information and their coverage guidelines. This assessment involves checking the medical necessity and potential alternatives to the proposed treatment.
Possible outcomes of your request
There are generally two outcomes following the evaluation: - **Approval**: If your request is approved, you can proceed with the prescribed treatment knowing it is covered by your insurance. You should receive detailed instructions on how to proceed. - **Denial**: In the case of a denial, the insurance company must provide a clear explanation for the decision. Understanding your rights is crucial, as you may have options to appeal the denial.
Troubleshooting common issues
It’s not uncommon to face issues when submitting your coverage determination request form. Delays might arise from incomplete submissions or the need for additional information from your healthcare provider. To resolve these issues, maintain communication with the insurance company and seek feedback on any required changes.
Understanding denials
Denials can happen for various reasons. Common causes include insufficient medical evidence, treatments deemed experimental, or services outside of the coverage network. If you face a denial, it is your right to appeal the decision. Collect further documentation and consult with your healthcare provider to strengthen your appeal.
Resources for assistance
When navigating the coverage determination process, it’s beneficial to have supportive resources at hand. Many insurance providers have dedicated customer service teams that can assist with queries regarding the coverage determination request form.
FAQs about the coverage determination request process
Understanding the coverage determination request form process often brings up several questions and concerns. For instance, if you find completion challenges, assistance can often be sought from healthcare providers or trained advocates. Furthermore, if a request is denied, it is indeed possible to appeal, and understanding the appeal process can empower you to seek the healthcare services you require.
Clarification on legal rights and procedures
Being aware of your legal rights within healthcare coverage determination is essential. Patients have the right to an appeal and should be informed about the procedures and timeframe for filing. Furthermore, insurers must provide you with the criteria used in making decisions. This transparency is critical for empowering patients in their healthcare journeys.
pdfFiller's role in simplifying the process
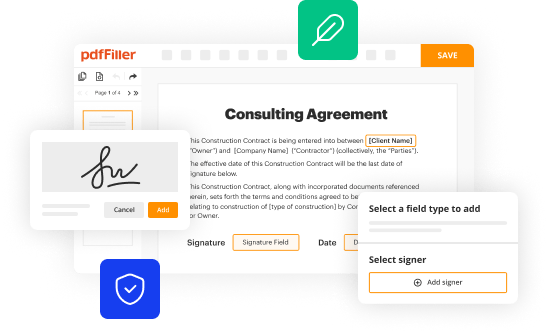
pdfFiller stands out as a powerful platform designed to streamline the entire process surrounding the coverage determination request form. Its tools allow users to seamlessly edit PDFs, eSign documents, and collaborate effectively on form management—all from a user-friendly, cloud-based environment. This capability significantly enhances the user experience by enabling flexibility and accessibility.
Benefits of using pdfFiller for coverage determination requests
The primary benefits of using pdfFiller include: - **Accessibility**: Forms can be accessed and completed from any device, making it convenient for both patients and providers. - **Collaboration**: Easily share documents among team members or with healthcare providers for quicker processing. - **eSigning**: Utilize the eSign feature to expedite form submission and enhance efficiency.
Latest news and updates
Staying informed on updates in healthcare policies and coverage determination is vital. Recently, Medicare has seen notable adjustments in its coverage policies, including increased provisions for telehealth services and updated guidelines on experimental treatments. Regularly checking informative articles and resources—like those available on pdfFiller—can ensure you remain knowledgeable and proactive in your healthcare decisions.






For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
How can I manage my coverage determination request form directly from Gmail?
How do I edit coverage determination request form online?
How do I fill out coverage determination request form on an Android device?
What is coverage determination request form?
Who is required to file coverage determination request form?
How to fill out coverage determination request form?
What is the purpose of coverage determination request form?
What information must be reported on coverage determination request form?
pdfFiller is an end-to-end solution for managing, creating, and editing documents and forms in the cloud. Save time and hassle by preparing your tax forms online.