Get the free daw penalty
Get, Create, Make and Sign daw penalty form
Editing daw penalty form online
Uncompromising security for your PDF editing and eSignature needs
How to fill out daw penalty form
How to fill out coverage determination request form
Who needs coverage determination request form?
Understanding the Coverage Determination Request Form
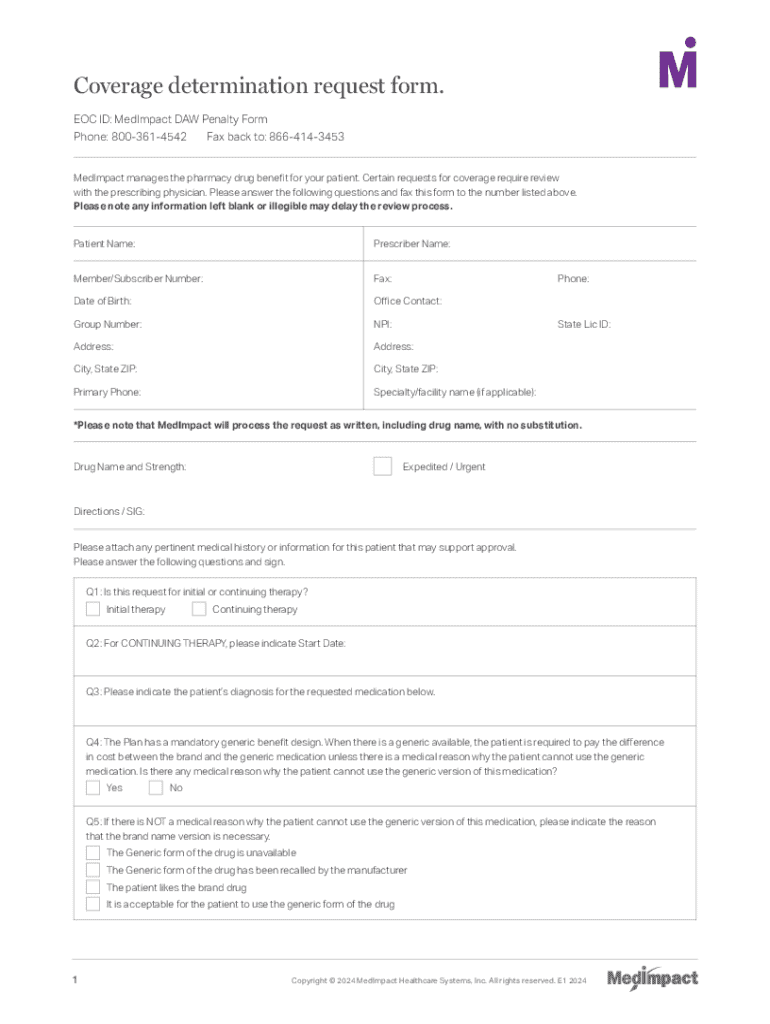
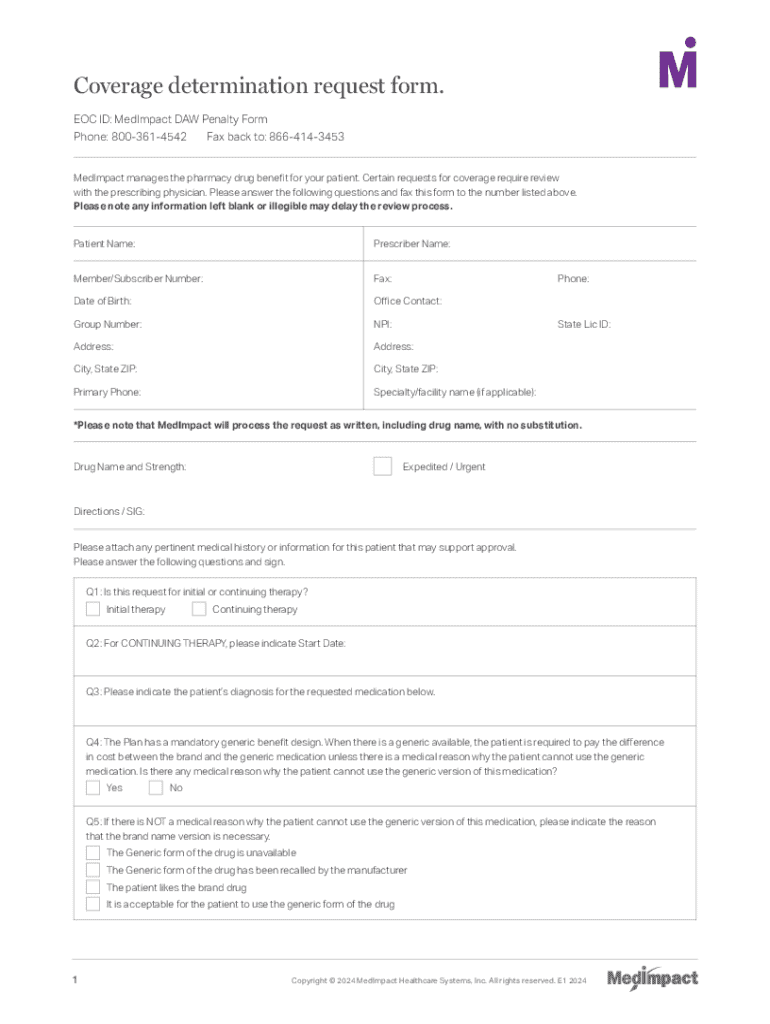
Overview of the coverage determination request form
The coverage determination request form serves as a crucial document in the healthcare system. Its primary purpose is to help patients and providers request approval from insurance providers for specific medical services or treatments. This form is essential for ensuring that patients receive the necessary care without unnecessary financial burden.
Understanding the significance of coverage determination is vital, as it directly impacts patient access to treatments and services. Coverage determination helps mitigate disputes regarding what is covered under a patient’s insurance plan, providing clarity and guidance on preventive care, procedures, and specialized therapies.
Understanding eligibility criteria
Not everyone can submit a coverage determination request form. Generally, the eligibility to submit the form includes patients, providers, and in some cases, caregivers. To streamline the submission process, knowing who is eligible is crucial in ensuring the form is filled out correctly.
Coverage requests can vary widely ranging from prescription drugs to specialized procedures. Potential requests might include advanced imaging studies, elective surgeries, or experimental treatments that the insurer needs to evaluate for coverage.
Step-by-step guide to completing the coverage determination request form
Completing the coverage determination request form effectively requires careful preparation and knowledge of the required information. Start by gathering necessary details about the patient, provider, and insurance coverage. This ensures that every needed criterion is met before submission.
Next, it's vital to fill out the form methodically. Each section has a specific purpose, detailing different aspects of the request. For instance, patient identification is crucial for matching the approval with the right individual.
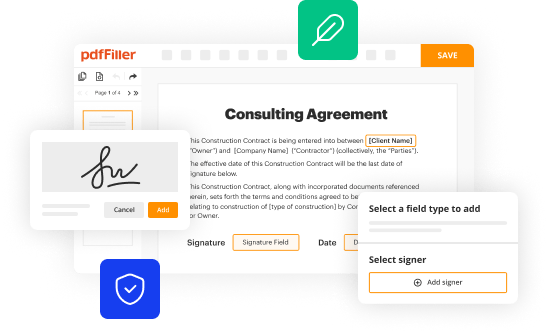
Common mistakes in filling out these forms include incorrect patient information and lack of supporting documentation. Always double-check that everything aligns with the patient’s health needs. To help visualize a correctly completed form, refer to online resources or sample templates available on helpful platforms like pdfFiller.
Interactive tools for managing coverage requests
In the digital age, managing coverage determination requests has become easier with interactive tools. Platforms such as pdfFiller not only provide templates for the coverage determination request form, but they also allow users to edit, store, and track their documents seamlessly.
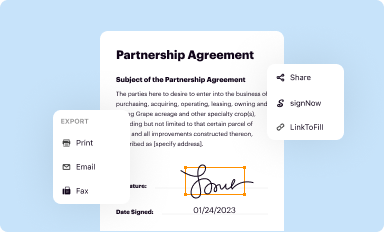
One of the key features is the eSignature integration that ensures faster approvals. With this tool, users can sign the document electronically, which helps expedite the process significantly.
Frequently asked questions (FAQs)
After submitting the coverage determination request form, many patients have questions about the next stages of the process. A common query involves the timeframe for processing requests, which can vary depending on the insurance provider. Typically, you can expect a response within a few days to a couple of weeks.
Additionally, in the event of a denial, it is essential to understand the appeals process. Knowing what to include in your appeal—such as additional documentation or a letter explaining the necessity of the treatment—can significantly influence the outcome.
Resources for understanding Medicare coverage determinations
For those on Medicare, understanding the specific policies surrounding coverage determinations is vital. Medicare uses a structured process to assess whether a particular service qualifies for coverage based on clinical necessity and the Medicare guidelines.
A comprehensive understanding of these policies can empower patients and providers to make informed decisions regarding treatment options. Resources from Medicare's website can guide you through specific coverage policies, common procedures requiring a prior authorization, and other related matters.
Best practices for submitting a successful coverage determination request
To increase the odds of a successful coverage determination request, it’s essential to include strong supporting documentation. This could be medical records, previous treatment histories, and a well-crafted letter from your healthcare provider detailing the medical necessity.
Clear communication with insurance providers can make a significant difference. Ensure that any interaction, whether via phone or email, is documented to create a paper trail. Following up is an often overlooked aspect of the process that can lead to expedited approvals.
Need help? Support and guidance
Navigating the complexities of coverage determination requests can often feel daunting. It's essential to know that various resources are available to assist you, including direct contact information for insurance providers and specialists who can offer personalized consultations.
Additionally, community forums can provide insights from fellow patients sharing their experiences and tips on handling requests. Engaging with these platforms can provide you confidence and support.
Current trends and news in coverage determination
The landscape of coverage determination is continually evolving, especially with reforms in healthcare regulations and insurance policies. Staying informed about recent updates is essential for both patients and healthcare providers to navigate these changes effectively.
Innovations in the coverage determination process, such as automated systems and artificial intelligence, are extending their presence in healthcare, aiming to simplify requests and make them more efficient.
Tools for tracking your coverage request
Utilizing technology to track your coverage request can significantly ease the process. Platforms like pdfFiller provide features that allow you to monitor the status of your submission and receive updates automatically.
These tools not only help manage requests but can also send reminders for follow-ups, ensuring that you stay informed throughout the coverage determination process and avoid potential delays.
Final thoughts
Completing a coverage determination request form can appear complex, but with the right tools and resources, it can be a smooth process. Platforms like pdfFiller provide the necessary support to navigate these challenges effectively.
Always stay informed about the best practices and emerging trends in coverage determination, helping you take proactive steps toward securing care when needed. Embrace the power of streamlined document management to enhance your healthcare experience.






For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
How can I send daw penalty form to be eSigned by others?
How do I complete daw penalty form on an iOS device?
Can I edit daw penalty form on an Android device?
What is coverage determination request form?
Who is required to file coverage determination request form?
How to fill out coverage determination request form?
What is the purpose of coverage determination request form?
What information must be reported on coverage determination request form?
pdfFiller is an end-to-end solution for managing, creating, and editing documents and forms in the cloud. Save time and hassle by preparing your tax forms online.