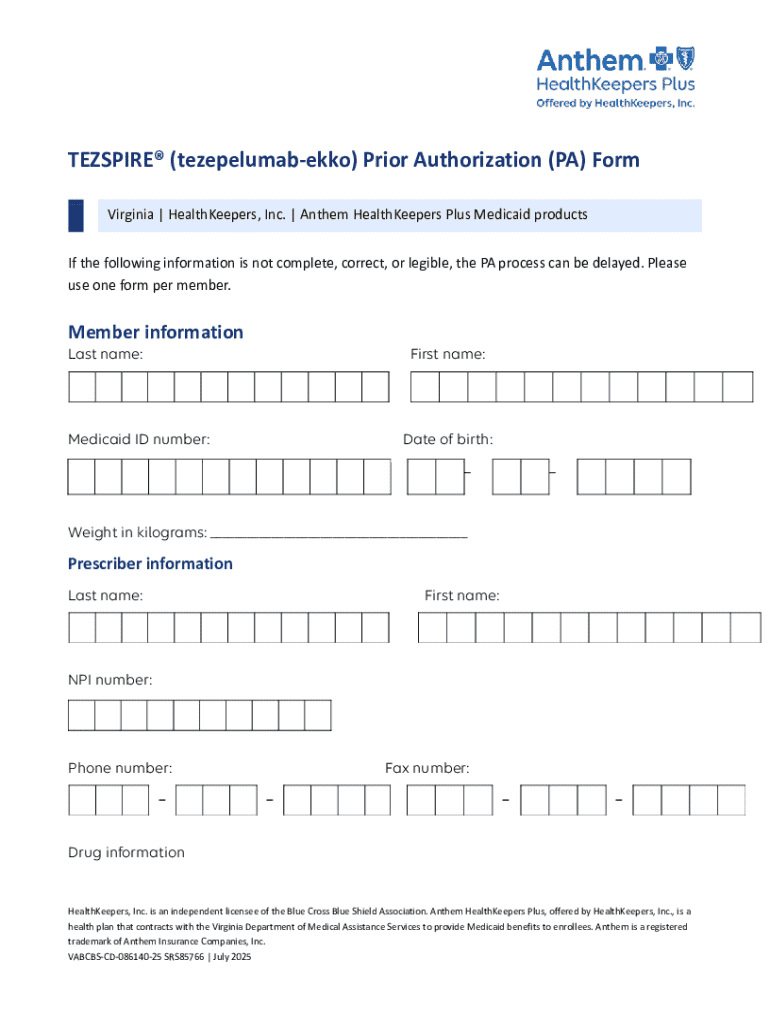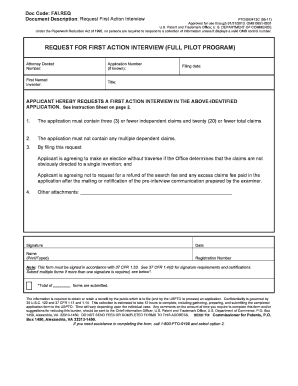
Get the free Tezspire® (tezepelumab-ekko) Prior Authorization (pa) Form
Get, Create, Make and Sign tezspire tezepelumab-ekko prior authorization
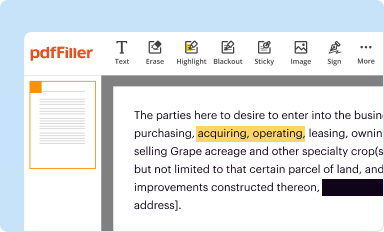
How to edit tezspire tezepelumab-ekko prior authorization online
Uncompromising security for your PDF editing and eSignature needs
How to fill out tezspire tezepelumab-ekko prior authorization
How to fill out tezspire tezepelumab-ekko prior authorization
Who needs tezspire tezepelumab-ekko prior authorization?
Tezspire Tezepelumab-Ekko Prior Authorization Form - How-to Guide
Understanding Tezspire and its purpose
Tezspire, also known as Tezepelumab-Ekko, is a novel biologic therapy specifically designed for the treatment of severe asthma. This medication functions by targeting a key pathway in the immune system, known as thymic stromal lymphopoietin (TSLP), to help control symptoms and reduce asthma exacerbations. Tezspire is generally indicated for patients aged 12 years and older who have a history of severe asthma that is inadequately controlled with standard therapies.
Prior authorization is crucial for Tezspire because it establishes medical necessity and ensures that the treatment aligns with the patient’s health plan guidelines. Insurers use prior authorization as a mechanism to determine eligibility for coverage before the medication is dispensed.
Why is a prior authorization form necessary?
The prior authorization process plays a vital role in healthcare. It helps health plans manage costs while ensuring patients receive appropriate treatments. By requiring healthcare providers to submit a prior authorization form for Tezspire, insurers can verify that the patient meets specific criteria for this specialty medication.
The benefits of obtaining approval before commencing treatment include reduced financial risks for patients, streamlined access to therapy, and fewer delays in care. Furthermore, securing prior authorization can assist healthcare providers in advocating for their patients' needs by closely aligning treatment interventions with insurance coverage policies.
Preparing to fill out the Tezspire prior authorization form
Before starting to fill out the Tezspire prior authorization form, it is essential to gather all the necessary information to ensure accuracy and completeness. Key patient details, such as the full name, date of birth, and insurance information, must be included. Additionally, having access to relevant medical history related to the asthma condition and any previous treatments can streamline the process.
Furthermore, including the physician’s information, such as credentials and contact details, is crucial as this determines who is requesting the prior authorization. This ensures the appropriate person is held responsible for adhering to follow-up communications with the insurance provider.
Understanding insurance requirements
When submitting a prior authorization form, it is essential to comprehend what information the insurance provider typically looks for, as criteria may vary. Many insurers require documentation that supports the diagnosis of severe asthma and evidence of prior treatments that have been ineffective.
Knowing the specific criteria for each insurance provider can significantly impact the success of your submission. Having a clear understanding allows you to prepare accordingly and anticipate any additional documentation that may be necessary.
Step-by-step guide to completing the Tezspire prior authorization form
Completing the Tezspire prior authorization form requires attention to detail. Each section of the form serves a specific purpose, and correct completion is paramount for swift approval.
In the Patient Information section, accurately filling out personal details is foundational. You should double-check that names are spelled correctly, and all relevant contact details are included. This information provides the first impression to the reviewer.
Clinical Information section
In the Clinical Information section, you’ll need to provide detailed insight into the patient’s condition—specifically symptoms of asthma severity, frequency of exacerbations, and any prior medication trials. This historical data substantiates the necessity of Tezspire.
Treatment Plan section
The Treatment Plan section should outline the expected duration of therapy and the anticipated outcomes. This demonstrates that a systematic approach is being taken to improve the patient's health status, which is appealing to the insurance provider.
Tips for success
To ensure a successful submission, avoid common pitfalls such as overlooking critical details or leaving sections blank. Clarity and legibility are crucial—use clear handwriting or digital submission to minimize errors. Furthermore, consider offering an explanation if the patient has specific needs that make Tezspire particularly appropriate for them.
Submitting the prior authorization form
Once you have completed the Tezspire prior authorization form, submitting it without delay is imperative. There are several submission methods available, including online submission through the insurer’s portal, faxing, or mailing the documents directly.
Each submission method has its guidelines. For online submissions, follow the specific instructions on the organization's website. If you choose fax or mail, it's advisable to check the insurer's requirements to ensure the form reaches the correct department.
Documentation to include with submission
Make sure to include any required supporting documents when you submit the prior authorization form. This often includes lab results that support the diagnosis, summaries of previous treatment responses, and any other necessary clinical evidence to bolster your request.
Importance of keeping records
It's crucial to keep thorough records of your submission. Make copies of the completed form and all supporting documents for your files. Tracking the submission status with the insurer is essential for following up effectively.
What to expect after submission
After submitting the prior authorization form, you may wonder what happens next. Most health plans have a standard turnaround time for reviews, which can vary by insurer; typically, you can expect to hear back within a week to ten days.
The outcome of your authorization request can result in an approval, which allows you to move forward with the treatment, or a denial, which may require a deeper look into the reasons provided by the insurer.
Approved: next steps to proceed with treatment
If approved, ensure you understand any requirements related to the pharmacy or treatment plan as stipulated by the insurance company. Typically, the next step is arranging for the medication to be dispensed.
Denied: understanding reasons and the appeals process
If denied, carefully review the reasons stated in the denial letter. Many denials occur due to lack of documentation or failure to meet specific criteria. Slightly escalating your knowledge about these reasons can be a pivotal first step in challenging the decision.
Contacting insurers for status updates
Effective communication with insurance representatives is paramount. Be prepared to provide your authorization request details when contacting them, as this can expedite getting an update on your request status.
Handling denials and appeals
Understanding how to manage denials can be critical in ensuring that you don't miss out on necessary treatments. Common reasons for the denial of the Tezspire prior authorization include insufficient clinical evidence supporting the necessity of the drug or failure to document previous treatments adequately.
To appeal a denial, start by crafting an effective appeal letter that clearly outlines the rationale behind the request for Tezspire. Ensure you include key documentation that substantiates the request, such as updated medical records or a summary from the prescribing physician.
Support resources available
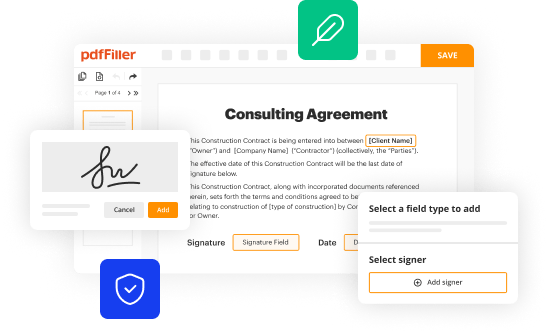
In terms of support, utilizing platforms like pdfFiller can streamline the documentation process while creating and managing necessary paperwork effectively. This service can provide templates and tools to help users better organize their appeal or create required documentation efficiently.
Conclusion and ongoing management
Maintaining regular follow-ups with insurance providers is essential as it ensures that any future needs for treatment can be adequately addressed. Regular communication can help preempt potential issues before they arise and provide a smoother pathway to necessary medications.
Leveraging pdfFiller for ongoing document management is beneficial not only now but in the future when further documentation may be required. With features that support seamless editing, signing, and collaborative tools, healthcare teams and patients can handle their healthcare forms with confidence and ease.






For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
How can I manage my tezspire tezepelumab-ekko prior authorization directly from Gmail?
How do I edit tezspire tezepelumab-ekko prior authorization on an Android device?
How do I complete tezspire tezepelumab-ekko prior authorization on an Android device?
What is tezspire tezepelumab-ekko prior authorization?
Who is required to file tezspire tezepelumab-ekko prior authorization?
How to fill out tezspire tezepelumab-ekko prior authorization?
What is the purpose of tezspire tezepelumab-ekko prior authorization?
What information must be reported on tezspire tezepelumab-ekko prior authorization?
pdfFiller is an end-to-end solution for managing, creating, and editing documents and forms in the cloud. Save time and hassle by preparing your tax forms online.