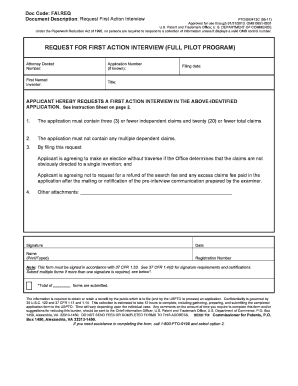
Get the free Prior Authorization Form
Get, Create, Make and Sign prior authorization form



Editing prior authorization form online
Uncompromising security for your PDF editing and eSignature needs
How to fill out prior authorization form

How to fill out prior authorization form
Who needs prior authorization form?
Understanding and Navigating the Prior Authorization Form
Understanding the prior authorization form
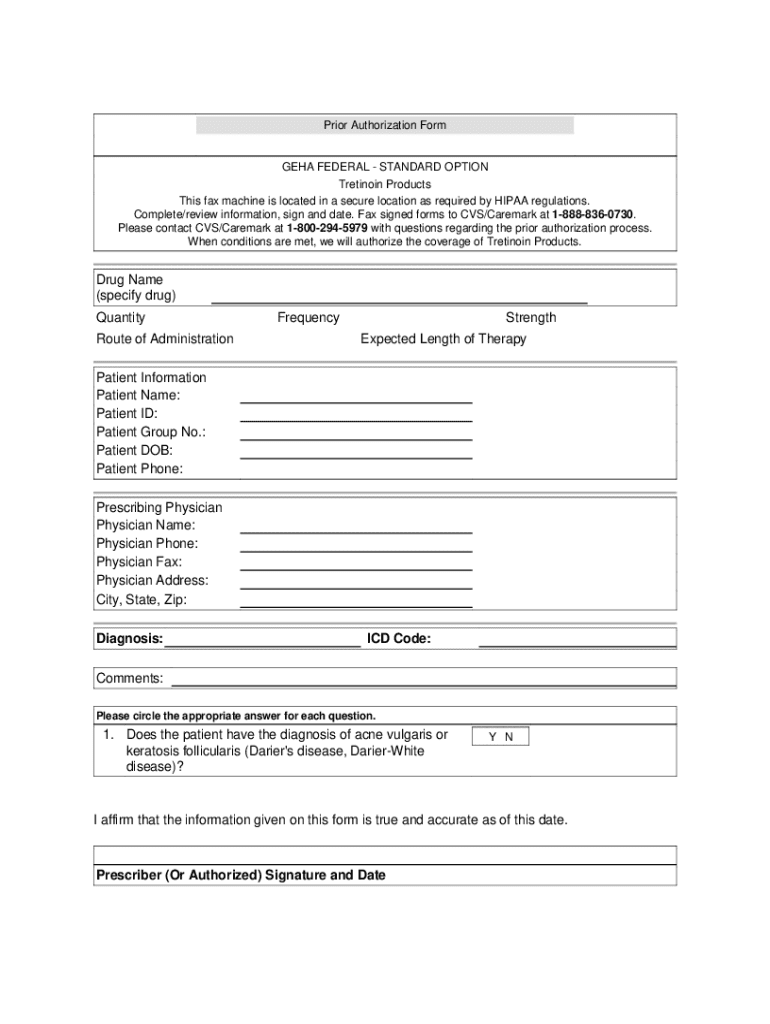
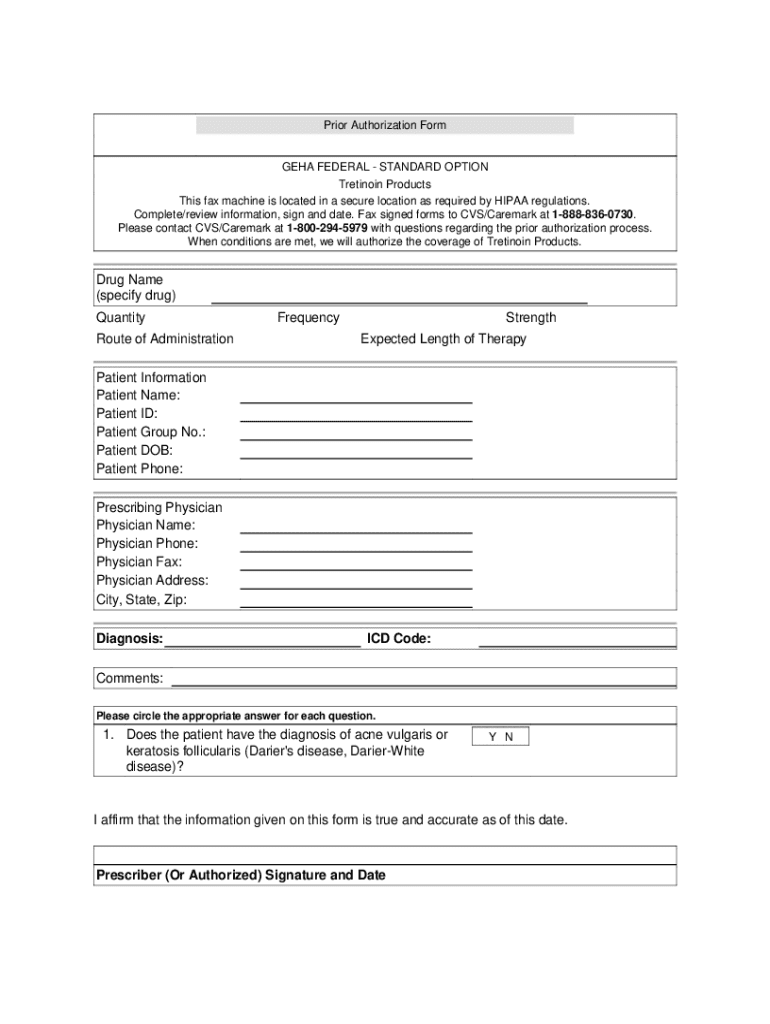
A prior authorization form is a request submitted to a health insurance company to obtain approval for a specific medical service, treatment, or prescription before it is provided to the patient. This process is critical in managing healthcare costs and ensuring that treatments are necessary and effective as recommended by medical professionals. The form plays a pivotal role in healthcare, as it safeguards the insurance company from covering unnecessary treatments while also assuring that patients receive appropriate care.
Prior authorization is usually mandated for high-cost treatments or procedures such as MRIs, surgeries, or specialty medications. It is a vital aspect of the healthcare system, guiding the approval process from both clinical and financial perspectives. Without prior authorization, patients may face significant out-of-pocket expenses for treatments deemed non-essential by their insurance providers, which underscores its importance.
Key components of a prior authorization form
When filling out a prior authorization form, it's crucial to include specific information to ensure accurate processing. The essential components of the form typically include personal information, patient information, insurance details, medical justifications, and provider information. These components collectively provide a comprehensive overview that assists insurance companies in making informed decisions.
Step-by-step guide to completing a prior authorization form
Completing a prior authorization form can seem daunting, but breaking it down into manageable steps makes the process straightforward. Firstly, gather all required information before starting to fill out the form. Having the necessary documents at hand will streamline the process and reduce the likelihood of errors.
Managing your prior authorization
Once you've submitted your prior authorization form, it's essential to manage the follow-up process effectively. Insurance providers generally provide a timeline for processing these requests, but delays can happen. It's recommended to follow up within a week or two if you haven't received a response.
Understanding insurance responses
After the submission, you'll receive one of three potential responses from your insurance provider: approved, denied, or pending. Understanding these responses allows you to take appropriate action.
Utilizing pdfFiller for your prior authorization form
pdfFiller is designed to enhance the experience of filling out prior authorization forms, providing a seamless interface for editing and customizing documents. The platform offers interactive tools that allow for real-time edits, making it easier for you to manage the intricacies of authorization requests.
Best practices for ensuring approval of prior authorization
To maximize the chances of receiving approval for your prior authorization request, follow best practices derived from industry experts. Thorough documentation is fundamental; providing adequate detailed information strengthens your case. Ensure that all necessary medical information, including support for the reasons for the request, is included.
Conclusion: Mastering the process of prior authorization
Mastering the prior authorization process involves understanding the nuances of documentation, timely follow-ups, and being prepared for various outcomes. Utilizing tools like pdfFiller simplifies the approach to managing these forms, enhancing efficiency through their cloud-based platform, allowing for edits, eSigning, and collaborative functionalities. For individuals and healthcare teams seeking to navigate this digital landscape seamlessly, pdfFiller provides an indispensable resource, making the prior authorization process more manageable and organized.






For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
How do I complete prior authorization form online?
Can I create an eSignature for the prior authorization form in Gmail?
How do I fill out prior authorization form on an Android device?
What is prior authorization form?
Who is required to file prior authorization form?
How to fill out prior authorization form?
What is the purpose of prior authorization form?
What information must be reported on prior authorization form?
pdfFiller is an end-to-end solution for managing, creating, and editing documents and forms in the cloud. Save time and hassle by preparing your tax forms online.