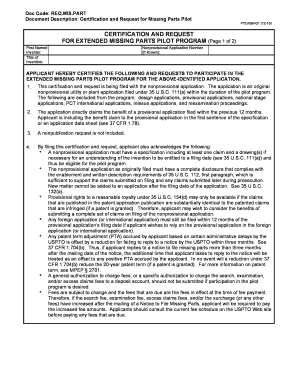
Get the free Jetrea Prior Authorization Form
Get, Create, Make and Sign jetrea prior authorization form



How to edit jetrea prior authorization form online
Uncompromising security for your PDF editing and eSignature needs
How to fill out jetrea prior authorization form

How to fill out jetrea prior authorization form
Who needs jetrea prior authorization form?
Comprehensive Guide to Jetrea Prior Authorization Form
Understanding the Jetrea prior authorization process
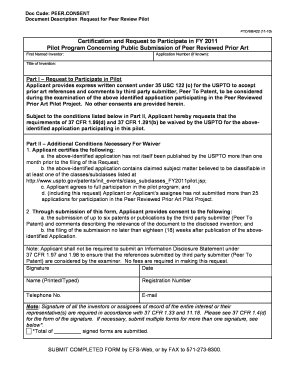
Prior authorization (PA) is a crucial process in healthcare, requiring healthcare providers to obtain approval from an insurance company before administering certain treatments or medications. This mechanism helps ensure that patients receive services that are medically necessary and within the scope of the plan. For treatments like Jetrea, which is used for managing symptomatic vitreomacular adhesion (VMA), navigating the PA landscape is essential for ensuring successful reimbursement.
Jetrea, a drug specifically tailored for VMA, necessitates approval from insurance plans to confirm it is an appropriate treatment option for patients. Each payer may have distinct requirements regarding documentation and clinical justification, making the prior authorization form a critical component in the treatment pathway. The key stakeholders in this process include patients, healthcare providers, and insurance companies, all of whom must collaborate effectively to facilitate a smooth authorization journey.
However, common challenges exist in securing authorization for Jetrea, including incomplete documentation, discrepancies in medical histories, or misinterpretations of payer requirements. These issues can delay treatment, causing frustration for both providers and patients. Understanding these dynamics is the first step toward effective management of the Jetrea prior authorization form.
Preparing to complete the Jetrea prior authorization form
Before you begin filling out the Jetrea prior authorization form, it's imperative to gather all necessary information to streamline the process. This includes detailed patient demographics such as age, gender, insurance account information, and contact details, all of which help set the context for treatment coverage. Additionally, specific nuances of the patient's medical history should be documented, particularly those directly related to vitreomacular conditions.
Healthcare providers should also prepare their credentials and any optional letters of medical necessity that support the treatment choice. These documents often play a pivotal role in the approval process and can expedite the administrative journey to receiving treatment.
Frequently requested supporting documents include clinical notes, imaging reports, and past treatment records, which substantiate claims for the medication's therapeutic need. Ensuring you have compiled these documents can significantly enhance the likelihood of a smooth submission.
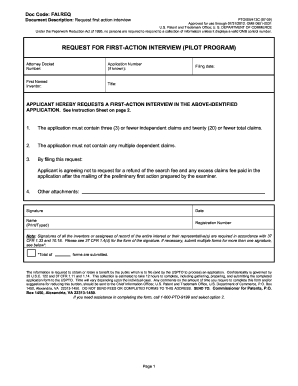
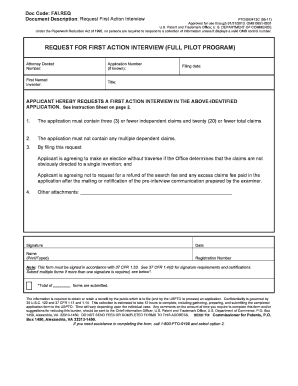
Step-by-step instructions for completing the Jetrea prior authorization form
Completing the Jetrea prior authorization form can be streamlined into three systematic steps, enhancing your chances of approval while minimizing delays. Here's how to approach this task effectively.
By adhering to these steps, healthcare providers can significantly reduce the chances of unnecessary follow-up requests and potential delays in treatment for patients.
Submission process for the Jetrea prior authorization form
Once you have completed the Jetrea prior authorization form, the next task is to submit it correctly. Typically, there are several options for submitting this form, either electronically via insurance company portals or via traditional mail.
Expect varying timelines depending on the insurer's processing policies, but it's prudent to follow up after submitting the form. Many organizations suggest checking back at least one week after submission to ensure everything is on track.
Managing the follow-up after submission
Following up after the submission of the Jetrea prior authorization form is vital. Standard practices usually involve receiving notifications regarding the status of the request either through phone calls or portal updates from the insurer. Companies typically inform providers once the request has been processed.
If the authorization request is denied, it’s crucial to understand the denial codes and their reasons. Common denials may stem from incomplete documentation or lack of medical necessity justification. In such cases, follow these best practices:
Effective follow-up and handling of denials can significantly improve the overall experience for both providers and patients seeking treatment with Jetrea.
Utilizing pdfFiller for Jetrea prior authorization form
pdfFiller introduces several features that enhance the user experience while completing the Jetrea prior authorization form. The cloud-based platform allows users to efficiently edit, eSign, and collaborate on essential documents from anywhere, ensuring teamwork and productivity.
The interactive tools available within pdfFiller assist in document tracking and management. Users can work collaboratively, sharing the form with other team members to facilitate input and ensure all areas are addressed before submission.
Moreover, pdfFiller offers secure storage for documents, making it easy to retrieve previous submissions and maintain thorough records as patients navigate their treatment processes.
Best practices for ensuring successful authorization
To maximize the chances of obtaining approval for the Jetrea prior authorization form, healthcare professionals should adhere to specific best practices. Open communication with insurance providers is paramount to understanding coverage requirements and avoiding documentation errors.
It's also crucial to stay updated on changes in medication policies, as insurance coverage can fluctuate and change with evolving medical guidelines. Consider these tips to bolster your submissions:
By implementing these strategies, healthcare providers will find greater success in navigating the complexities surrounding prior authorizations for Jetrea.
Alternative solutions and considerations
In exploring treatment options for conditions like VMA, it’s beneficial to consider alternatives to Jetrea. Other therapies may present viable options depending on individual patient needs, and understanding coverage for these alternatives can be equally crucial.
Discussing these treatments openly with healthcare providers can shed light on additional pathways that may be covered under patients' existing insurance plans. It is essential to weigh options thoughtfully, considering factors such as efficacy, side effects, and potential insurance coverage.
Ultimately, exploring a range of treatment possibilities in consultation with healthcare professionals can ensure patients receive optimal care tailored to their unique situations.
Patient resources and support networks
Patients undergoing treatment for conditions like VMA may require additional support beyond clinical solutions. Several organizations exist to offer assistance, educational resources, and a community for those navigating similar experiences.
Online communities can be especially valuable for sharing experiences and advice regarding treatment and coverage issues. Additionally, patient advocate services can provide personalized assistance with navigating the complexities of prior authorization and treatment decisions.
Building a supportive network can alleviate some burdens during treatment and empower patients to make informed decisions regarding their care.
Footer links
Utilize pdfFiller's platform for a seamless experience with the Jetrea prior authorization form. Explore quick links to related resources, contact information for assistance with Jetrea forms, and valuable insights into terms of use and privacy policy.






For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
How do I modify my jetrea prior authorization form in Gmail?
Can I sign the jetrea prior authorization form electronically in Chrome?
How do I fill out the jetrea prior authorization form form on my smartphone?
What is jetrea prior authorization form?
Who is required to file jetrea prior authorization form?
How to fill out jetrea prior authorization form?
What is the purpose of jetrea prior authorization form?
What information must be reported on jetrea prior authorization form?
pdfFiller is an end-to-end solution for managing, creating, and editing documents and forms in the cloud. Save time and hassle by preparing your tax forms online.