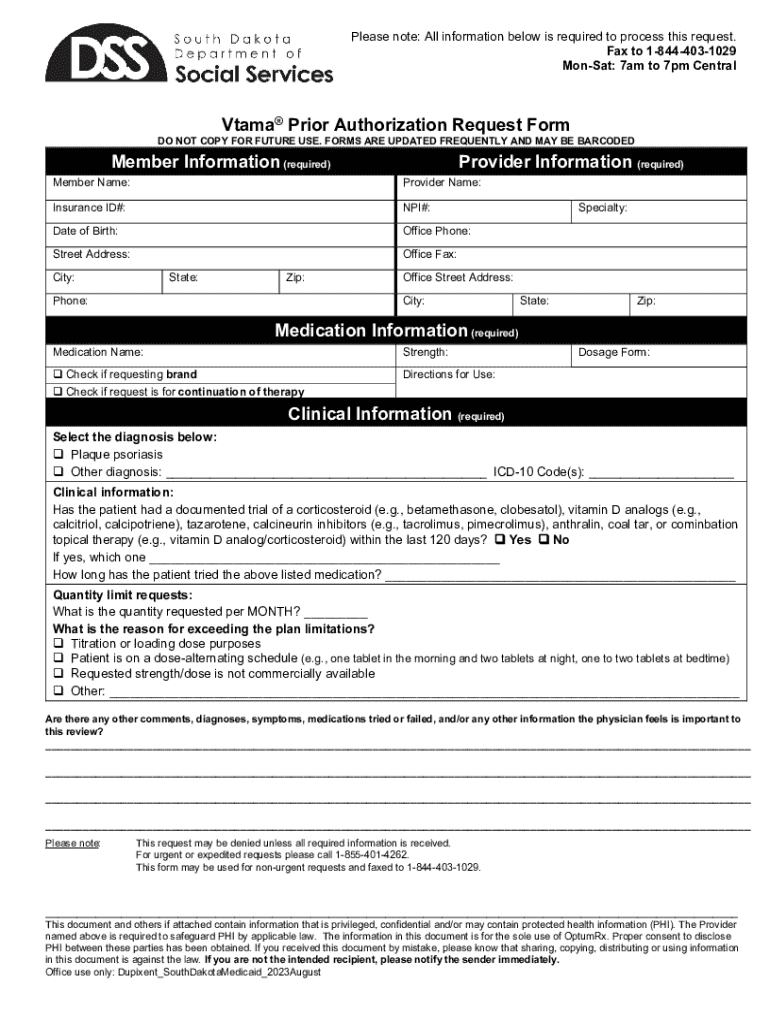
Get the free Vtama® Prior Authorization Request Form
Get, Create, Make and Sign vtama prior authorization request



How to edit vtama prior authorization request online
Uncompromising security for your PDF editing and eSignature needs
How to fill out vtama prior authorization request

How to fill out vtama prior authorization request
Who needs vtama prior authorization request?
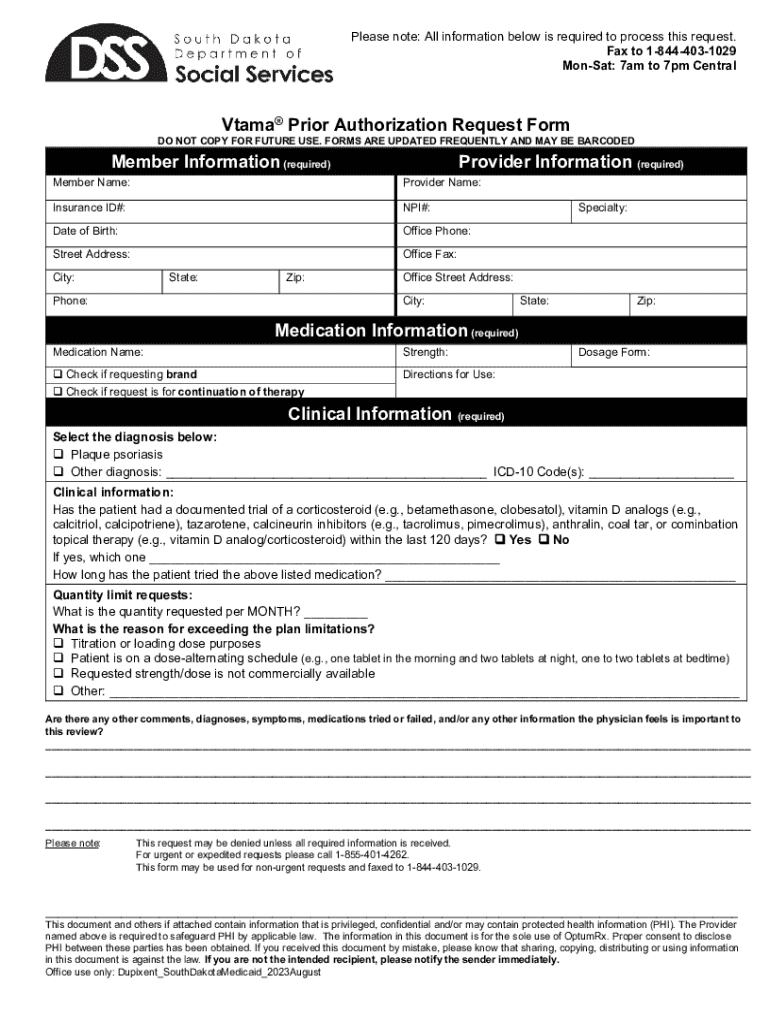
A Comprehensive Guide to the VTAMA Prior Authorization Request Form
Understanding the VTAMA prior authorization process
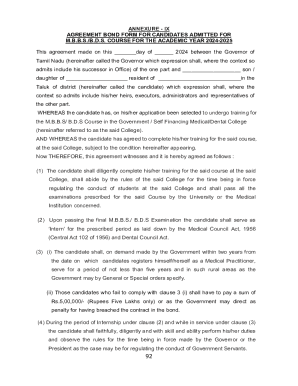
Prior authorization is a critical step in the healthcare process that requires healthcare providers to obtain approval from insurance companies before a specific treatment or medication can be administered. This process ensures that prescribed treatments align with patients' clinical needs and the insurance's coverage policies.
In the case of VTAMA, a medication used to treat plaque psoriasis, the prior authorization process is vital in determining eligibility and ensuring that patients can benefit from the treatment without unnecessary delays. VTAMA has been developed for patients who require topical treatments to manage their condition effectively.
Who needs to submit a VTAMA prior authorization request?
The submission of a VTAMA prior authorization request primarily falls on healthcare providers, including dermatologists and primary care physicians, who prescribe the medication. They must ensure their patients meet the eligibility criteria set forth by insurance providers.
Eligibility criteria can include factors such as the patient’s age, previous treatments attempted, and the severity of their psoriasis. Additionally, healthcare providers must familiarize themselves with individual insurance policies, which may vary significantly regarding specific coverage and requirements for VTAMA.
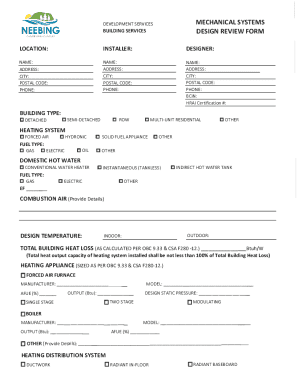
Step-by-step guide to completing the VTAMA prior authorization request form
Completing the VTAMA prior authorization request form involves several key steps to ensure that submissions are accurate and complete. Here’s a detailed look at each step:
Interactive tools for managing your VTAMA prior authorization request
Using tools available on pdfFiller can significantly enhance your experience managing the VTAMA prior authorization request. With pdfFiller’s editing capabilities, users can easily customize documents to meet specific requirements.
The platform includes eSignature integration to expedite the approval process and offers collaborative features that enable multiple team members to contribute to the form submission efficiently. This collaboration ensures that all relevant information is accounted for and can streamline the authorization process.
Potential outcomes of your prior authorization request
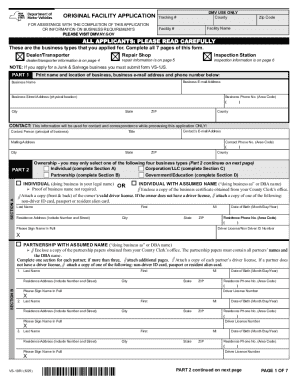
Once the VTAMA prior authorization request has been submitted, several outcomes may occur. Typically, patients can expect a response relatively quickly, depending on the insurance company’s processing times.
Approval notifications will usually come via the healthcare provider who submitted the form. If the request is denied, it is essential to understand the steps for reconsideration and how to navigate the appeals process effectively.
FAQs about VTAMA prior authorization
As with any healthcare process, there tends to be confusion surrounding the VTAMA prior authorization. Common questions include how to fill out the form correctly and what to do if the request is lost in the system.
Healthcare providers and patients can benefit from familiarizing themselves with the most frequently asked questions regarding the authorization process to mitigate concerns and ensure smooth submissions. Additional resources for further assistance are also available through healthcare providers and insurance companies.
Patient support and resources
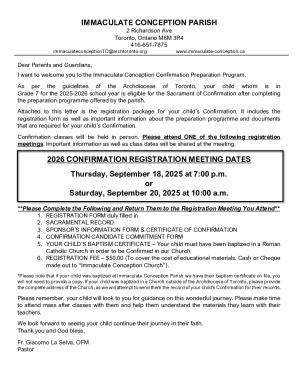
Patients prescribed VTAMA have access to a variety of support resources. This includes educational brochures that outline treatment options and potential savings opportunities for those dealing with out-of-pocket expenses.
Additionally, there is support available for patients who need direct assistance or wish to speak with a representative regarding their prescription and prior authorization process. This can help alleviate concerns during treatment.
Related forms and additional tools
In addition to the VTAMA prior authorization request form, there are several other prior authorization forms healthcare providers may need to familiarize themselves with, depending on the medications they prescribe.
Having access to downloadable resources ensures that all necessary forms can be completed efficiently. pdfFiller offers various templates to streamline this process, catering to different healthcare needs.
Staying informed: recent updates on VTAMA and prior authorization policies
Regulatory changes affecting prior authorizations are common. Healthcare providers must stay up-to-date with any shifts in insurance policies that could impact patient access to VTAMA. These changes can include new requirements for documentation or differing approval timelines.
Awareness of these updates can help medical professionals guide their patients effectively through the authorization landscape, ensuring treatments remain accessible and timely.
Testimonials and success stories
Patient success stories highlight the essential role that proper prior authorization plays in ensuring access to VTAMA. Numerous individuals have reported positive outcomes after receiving timely approvals for their treatment.
These testimonials serve not only to inform prospective patients about potential benefits but also to inspire confidence in healthcare providers managing the authorization process.






For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
How can I send vtama prior authorization request for eSignature?
How do I make changes in vtama prior authorization request?
How do I fill out the vtama prior authorization request form on my smartphone?
What is vtama prior authorization request?
Who is required to file vtama prior authorization request?
How to fill out vtama prior authorization request?
What is the purpose of vtama prior authorization request?
What information must be reported on vtama prior authorization request?
pdfFiller is an end-to-end solution for managing, creating, and editing documents and forms in the cloud. Save time and hassle by preparing your tax forms online.